Abstract
Mini Review
Stage and symptoms of bipolar disorders
Gudisa Bereda*
Published: 06 April, 2022 | Volume 6 - Issue 1 | Pages: 007-010
Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental disorder that causes unusual shifts in mood, energy, activity levels, concentration, and the ability to carry out day-to-day tasks. During mood swings, there may be features of psychosis (delusions and hallucinations) that are mood-congruent. Although psychotic symptoms are seen only in a minority of patients, they explain the early terminology of manic–depressive psychosis. Stage 1a is defined as mild or non-specific symptoms of mood disorder and intervened as formal mental health literacy; family psychoeducation; substance abuse reduction; cognitive behavioral therapy. Euphoric means the experience of pleasure or excitement and intense feelings of well-being and happiness. Certain natural rewards and social activities, such as aerobic exercise, laughter, listening to or making music, and dancing, can induce a state of euphoria. Racing thoughts are consistent, persistent, often intrusive thoughts that come in rapid succession. There is a direct link between depression and anxiety and racing thoughts. Whereas jumping from topic to topic as in the flight of ideas can be observed by others, ascertainment of racing thoughts requires asking the child whether his or her thoughts seem to be going too fast.
Read Full Article HTML DOI: 10.29328/journal.ida.1001030 Cite this Article Read Full Article PDF
Keywords:
Bipolar disorders; Stage; Symptoms
References
- Brickman HM, Fristad MA. Psychosocial Treatments for Bipolar Disorder in Children and Adolescents. Annu Rev Clin Psychol. 2022. 18: 20.1–20.37.
- Lee H, Han D, Rhee SJ, Kim J, Lee Y, et al. Alterations in blood proteins in the prodromal stage of bipolar II disorders. Sci Rep. 2022; 12: 3174. PubMed: https://pubmed.ncbi.nlm.nih.gov/35210508/
- Göteson A, Isgren A, Sparding T, Holmén-Larsson J, Jakobsson J, et al. A serum proteomic study of two case-control cohorts identifies novel biomarkers for bipolar disorder. Translational Psychiatry. 2022: 12: 55.
- Ching CRK, Hibar DP, Gurholt TP, Nunes A, Thomopoulos SI, et al. What we learn about bipolar disorder from large-scale neuroimaging: Findings and future directions from the ENIGMA Bipolar Disorder Working Group. Hum Brain Mapp. 2022; 43: 56–82. PubMed: https://pubmed.ncbi.nlm.nih.gov/32725849/
- Post RM, Grunze H. The Challenges of Children with Bipolar Disorder. Medicina. 2021; 57: 601. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8230664/
- Duffy A, Goodday S, Keown-Stoneman C, Grof P. The Emergent Course of Bipolar Disorder: Observations Over Two Decades from the Canadian High-Risk Offspring Cohort. Am J Psychiatry. 2019; 176: 720–729. PubMed: https://pubmed.ncbi.nlm.nih.gov/30525908/
- Hafeman DM, Rooks B, Merranko J, Liao F, Gill MK, et al. Lithium Versus Other Mood-Stabilizing Medications in a Longitudinal Study of Youth Diagnosed with Bipolar Disorder. J Am Acad Child. Adolesc. Psychiatry. 2020; 59: 1146–1155. PubMed: https://pubmed.ncbi.nlm.nih.gov/31369795/
- Findling RL, McNamara NK, Pavuluri M, Frazier JA, Rynn M, et al. Lithium for the Maintenance Treatment of Bipolar I Disorder: A Double-Blind, Placebo-Controlled Discontinuation Study. J Am Acad Child Adolesc Psychiatry. 2019; 58: 287–296.e284. PubMed: https://pubmed.ncbi.nlm.nih.gov/30738555/
- Velosa J, Delgado A, Finger E, Berk M, Kapczinski F, et al. Risk of dementia in bipolar disorder and the interplay of lithium: A systematic review and meta-analyses. Acta Psychiatr Scand. 2020; 141: 510–521. PubMed: https://pubmed.ncbi.nlm.nih.gov/31954065/
- Anmella G, Fico G, Lotfaliany M, Hidalgo-Mazzei D, Soto-Angona Ó, et al. Risk of cancer in bipolar disorder and the potential role of lithium: International collaborative systematic review and meta-analyses. Neurosci Biobehav Rev. 2021; 126: 529–541. PubMed: https://pubmed.ncbi.nlm.nih.gov/33831461/
- Raison CL, Siu C, Pikalov A, Tocco M, Loebel A. C-reactive protein and response to lurasidone treatment in children and adolescents with bipolar I depression: Results from a placebo-controlled trial. Brain Behav Immun. 2020; 84: 269–274. PubMed: https://pubmed.ncbi.nlm.nih.gov/31857217/
- Post RM, Goldstein BI, Birmaher B, Findling RL, Frey BN, et al. Toward prevention of bipolar disorder in at-risk children: Potential strategies ahead of the data. J Affect Disord. 2020; 272: 508–520. PubMed: https://pubmed.ncbi.nlm.nih.gov/32553395/
- Wang G, Wu L, Su H, Feng X, Shi M, et al. Association of urinary matrix metalloproteinase 7 levels with incident renal flare in lupus nephritis. Arthritis Rheumatol. 2021; 73: 265–275. PubMed: https://pubmed.ncbi.nlm.nih.gov/32892475/
- Fu H, Zhou D, Zhu H, Liao J, Lin L, et al. Matrix metalloproteinase-7 protects against acute kidney injury by priming renal tubules for survival and regeneration. Kidney Int. 2019; 95: 1167–1180. PubMed: https://pubmed.ncbi.nlm.nih.gov/30878215/
- Chen S, Jiang H, Hou Z, Yue Y, Zhang Y, et al. Higher serum VGF protein levels discriminate bipolar depression from major depressive disorder. J Neurosci Res. 2019; 97: 597–606. PubMed: https://pubmed.ncbi.nlm.nih.gov/30575991/
- Rhee SJ, Han D, Lee Y, Kim H, Lee J, et al. Comparison of serum protein profiles between major depressive disorder and bipolar disorder. BMC Psychiatry. 2020; 20: 145. PubMed: https://pubmed.ncbi.nlm.nih.gov/32245436/
- Jeppesen P, Wolf RT, Nielsen SM, Christensen R, Plessen KJ, et al. Effectiveness of Transdiagnostic Cognitive-Behavioral Psychotherapy Compared with Management as Usual for Youth with Common Mental Health Problems: A Randomized Clinical Trial. JAMA Psychiatry. 2021; 78: 1–12. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7758821/
- Smirnova L, Seregin A, Boksha I, Dmitrieva E, Simutkin G, et al. The difference in serum proteomes in schizophrenia and bipolar disorder. BMC Genomics. 2019; 20: 535–535. PubMed: https://pubmed.ncbi.nlm.nih.gov/31291891/
- Pascual-Sánchez A, Jenaro C, Montes-Rodríguez JM. Quality of life in euthymic bipolar patients: a systematic review and meta-analysis. J Affect Disord. 2019; 255: 105–115. PubMed: https://pubmed.ncbi.nlm.nih.gov/31150940/
- Munkholm K, Vinberg M, Pedersen BK, Poulsen HE, Ekstrøm CT, et al. A multisystem composite biomarker as a preliminary diagnostic test in bipolar disorder. Acta Psychiatr Scand. 2019; 139: 227–236. PubMed: https://pubmed.ncbi.nlm.nih.gov/30383306/
- Brandon M, Greenwell BCB. Variable importance plots—an introduction to the vip package. R J. 2020; 12: 343–366.
- Wiener CD, Moreira FP, Portela LV, Strogulski NR, Lara DR, et al. Interleukin-6 and Interleukin-10 in mood disorders: a population-based study. Psychiatry Res. 2019; 273: 685–689. PubMed: https://pubmed.ncbi.nlm.nih.gov/31207853/
- Barbosa IG, Ferreira RA, Rocha NP, Mol GC, da Mata Chiaccjio Leite F, et al. Predictors of cognitive performance in bipolar disorder: The role of educational degree and inflammatory markers. J Psychiatr Res. 2018; 106: 31–37. PubMed: https://pubmed.ncbi.nlm.nih.gov/30261412/
- Mørch RH, Dieset I, Færden A, Reponen EJ, Hope S, et al. Inflammatory markers are altered in severe mental disorders independent of comorbid cardiometabolic disease risk factors. Psychol Med. 2019; 49: 1749–1757. PubMed: https://pubmed.ncbi.nlm.nih.gov/30688187/
- Poletti S, Vai B, Mazza MG, Zanardi R, Lorenzi C, et al. A peripheral inflammatory signature discriminates bipolar from unipolar depression: a machine learning approach. Prog Neuropsychopharmacol Biol Psychiatry. 2021; 105: 110136. PubMed: https://pubmed.ncbi.nlm.nih.gov/33045321/
- Sahin B, Inanli I, Calıskan AM, Uysal S. Chitinase-3-like protein 1 levels in bipolar disorder. Saudi Med J. 2019; 40: 26–32. PubMed: https://pubmed.ncbi.nlm.nih.gov/30617377/
- McIntyre RS. Is obesity changing the phenotype of bipolar disorder from predominately euphoric toward mixed presentations? Bipolar Disord. 2018; 20: 685–686. PubMed: https://pubmed.ncbi.nlm.nih.gov/30412345/
- Burdick KE, Millett CE, Bonnín CDM, Bowie CR, Carvalho AF, et al. The International Consortium Investigating Neurocognition in Bipolar Disorder (ICONIC-BD). Bipolar Disord. 2019; 21: 6–10. PubMed: https://pubmed.ncbi.nlm.nih.gov/30720913/
- Altshuler LL, Sugar CA, McElroy SL, Calimlim B, Gitlin M, et al. Switch Rates During Acute Treatment for Bipolar II Depression With Lithium, Sertraline, or the Two Combined: A Randomized Double-Blind Comparison. Am J Psychiatry. 2017; 174: 266–276. PubMed: https://pubmed.ncbi.nlm.nih.gov/28135846/
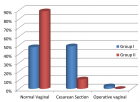
Figures:
Similar Articles
-
Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and GermanyJochen Hardt*,Lisa Weyer,Malgorzata Dragan,Wilfried Laubach. Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and Germany. . 2017 doi: 10.29328/journal.hda.1001003; 1: 015-022
-
Problems shared in psychiatry helpline of a teaching hospital in eastern Nepal during COVID-19 pandemic lockdownDhana Ratna Shakya*. Problems shared in psychiatry helpline of a teaching hospital in eastern Nepal during COVID-19 pandemic lockdown. . 2020 doi: 10.29328/journal.ida.1001017; 4: 037-039
-
Burden and depressive symptoms in health care residents at COVID-19: A preliminary reportDaniela Betinassi Parro-Pires*,Sérgio Henrique de C Matias Barros,Fernanda Sabina HD Araújo,Daniel Zandoná Santos,Luiz Antônio Nogueira-Martins,Vanessa de Albuquerque Citero. Burden and depressive symptoms in health care residents at COVID-19: A preliminary report. . 2021 doi: 10.29328/journal.ida.1001024; 5: 005-008
-
Depression and anxiety in patients with suspected renal artery stenosisLudvig Hallberg*,Anders Gottsater,Anders Isaksson,Asa Westrin. Depression and anxiety in patients with suspected renal artery stenosis. . 2021 doi: 10.29328/journal.ida.1001026; 5: 009-015
-
Observation of telepsychiatry service in a teaching hospital of eastern Nepal during COVID-19 pandemicDhana Ratna Shakya*. Observation of telepsychiatry service in a teaching hospital of eastern Nepal during COVID-19 pandemic. . 2021 doi: 10.29328/journal.ida.1001027; 5: 025-028
-
Stage and symptoms of bipolar disordersGudisa Bereda*. Stage and symptoms of bipolar disorders. . 2022 doi: 10.29328/journal.ida.1001030; 6: 007-010
-
Predicting physical symptoms through expressions of loneliness and anxiety in individuals utilizing social media during SARS-CoV-2Vasiliki Georgoulas-Sherry*. Predicting physical symptoms through expressions of loneliness and anxiety in individuals utilizing social media during SARS-CoV-2. . 2022 doi: 10.29328/journal.ida.1001031; 6: 011-017
-
Identifying mothers experiencing emotional distress in the neonatal intensive care unit. Application of PPTSD questionnaire in a Greek NICU populationKarkani Anastasia*,Theodoraki Martha,Paraskeva Natasa,Kouros Pavlos Aristidis,Pantelis Perdikaris,Rosenblum Ouriel,Mazet Philippe. Identifying mothers experiencing emotional distress in the neonatal intensive care unit. Application of PPTSD questionnaire in a Greek NICU population. . 2022 doi: 10.29328/journal.ida.1001033; 6: 025-031
-
Clinical and immunological characteristics of depressive patients with a clinical high risk of schizophreniaOmelchenko MA,Zozulya SA,Kaleda VG,Klyushnik TP*. Clinical and immunological characteristics of depressive patients with a clinical high risk of schizophrenia. . 2023 doi: 10.29328/journal.ida.1001034; 7: 001-003
-
Is binge watching among medical students associated with depression and anxiety?Meriem Hamza*,Soumeyya Halayem,Imène Jraidi,Myriam Boudali,Asma Bouden,Ahlem Belhadj. Is binge watching among medical students associated with depression and anxiety?. . 2023 doi: 10.29328/journal.ida.1001035; 7: 004-010
Recently Viewed
-
Obstructive Pyelonephritis Due to Postoperative Ureteral Stricture: A Case ReportAyoub Mamad*,Mohammed Amine Elafari,Mohammed Amine Bibat,Midaoui Moncef,Amine Slaoui,Tarik Karmouni,Abdelatif Koutani,Khalid Elkhader. Obstructive Pyelonephritis Due to Postoperative Ureteral Stricture: A Case Report. J Clin Med Exp Images. 2026: doi: 10.29328/journal.jcmei.1001039; 10: 003-005
-
The motivational factors and adverse events experienced by healthy volunteers donating bone marrow for researchMirella Ejiugwo,Georgina Shaw,Frank Barry,Janusz Krawczyk,Veronica McInerney*. The motivational factors and adverse events experienced by healthy volunteers donating bone marrow for research. Int J Bone Marrow Res. 2019: doi: 10.29328/journal.ijbmr.1001010; 2: 089-096
-
Primary myelofibrosis is not primary anymore since the discovery of MPL515 and CALR mutations as driver causes of mono-linear megakaryocytic and dual megakaryocytic granulocytic myeloproliferation and secondary myelofibrosisJan Jacques Michiels*,Hendrik De Raeve. Primary myelofibrosis is not primary anymore since the discovery of MPL515 and CALR mutations as driver causes of mono-linear megakaryocytic and dual megakaryocytic granulocytic myeloproliferation and secondary myelofibrosis. Int J Bone Marrow Res. 2019: doi: 10.29328/journal.ijbmr.1001003; 2: 018-026
-
Pure Erythroid Leukemia: The Sole Acute Erythroid LeukemiaFauzia Shafi Khan*,Khalid Mahmood,Alia Ahmad. Pure Erythroid Leukemia: The Sole Acute Erythroid Leukemia. Int J Bone Marrow Res. 2017: doi: 10.29328/journal.ijbmr.1001001; 1: 001-005
-
European Clinical Laboratory, Molecular and Pathological (ECMP) criteria for prefibrotic JAK2V617F-Thrombocythemia and Polycythemia Vera versus MPL515- and CALR-Thrombocythemia and Myelofibrosis: From Dameshek to Michiels 1950-2018Jan Jacques Michiels*,Zwi Berneman,Wilfried Schroyens,Fibo W J ten Kate,King Lam,Hendrik De Raeve. European Clinical Laboratory, Molecular and Pathological (ECMP) criteria for prefibrotic JAK2V617F-Thrombocythemia and Polycythemia Vera versus MPL515- and CALR-Thrombocythemia and Myelofibrosis: From Dameshek to Michiels 1950-2018. Int J Bone Marrow Res. 2019: doi: 10.29328/journal.ijbmr.1001002; 2: 001-017
Most Viewed
-
Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trialSathit Niramitmahapanya*,Preeyapat Chattieng,Tiersidh Nasomphan,Korbtham Sathirakul. Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trial. Ann Clin Endocrinol Metabol. 2023 doi: 10.29328/journal.acem.1001026; 7: 00-007
-
Physical Performance in the Overweight/Obesity Children Evaluation and RehabilitationCristina Popescu, Mircea-Sebastian Șerbănescu, Gigi Calin*, Magdalena Rodica Trăistaru. Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001030; 8: 004-012
-
Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging PresentationKarthik Baburaj*, Priya Thottiyil Nair, Abeed Hussain, Vimal MV. Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging Presentation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001029; 8: 001-003
-
Exceptional cancer responders: A zone-to-goDaniel Gandia,Cecilia Suárez*. Exceptional cancer responders: A zone-to-go. Arch Cancer Sci Ther. 2023 doi: 10.29328/journal.acst.1001033; 7: 001-002
-
The benefits of biochemical bone markersSek Aksaranugraha*. The benefits of biochemical bone markers. Int J Bone Marrow Res. 2020 doi: 10.29328/journal.ijbmr.1001013; 3: 027-031

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."