Abstract
Brief Communication
Problems shared in psychiatry helpline of a teaching hospital in eastern Nepal during COVID-19 pandemic lockdown
Dhana Ratna Shakya*
Published: 27 April, 2020 | Volume 4 - Issue 1 | Pages: 037-039
COVID-19 pandemic soon apparently proved to be havoc and a great stressor. During such a stressful time, mental health is in threat. Here, we intend to review the presenting problems/ symptoms as shared in psychiatry helpline of a Teaching Hospital in eastern Nepal during the second week of lockdown and to reflect on to emotional, including mood problems.
It is an institute based period observation noted for all psychiatry helpline calls during 1 week of lockdown days of COVID-19. Their concerns and problems were listened and symptoms clarified by a consultant psychiatrist to help them as far as possible through the telephonic conversation. Maintaining the confidentiality, basic information were noted down in a semi-structured proforma to record certain socio-demographic and clinical information (including mood and other emotional symptoms).
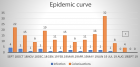
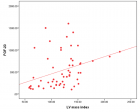
We received 102 helpline calls of 60 clients for psychiatry in 1 week, from 14 districts. More patients being discussed were males (35/60), average age being 34.15 (15 - 70) years. More patients were regular follow-up cases with some new issues (24/60) and 18/60 each were new clients and regular follow-up cases. Majority had exacerbated symptoms in the wake of COVID-19 as: emotional (47/60; mood 24/60, anxiety/worry 23/60) symptoms along with disturbed sleep (32/60); treatment/service issues (31/60) and changed routines. Most common mental problems were Bipolar affective disorder, Psychosis, Anxiety and Depression and advices included Antipsychotics, Benzodiazepines, Antidepressants, along with some Psycho-education. Most common concerns were about OPD service, worsening symptoms and local unavailability of medicines. Many had mood and emotional symptoms in this stressful time, both simple amenable to telephonic advices and severe requiring to be called to emergency service.
Read Full Article HTML DOI: 10.29328/journal.ida.1001017 Cite this Article Read Full Article PDF
Keywords:
COVID-19; Emotional; Psychiatry helpline; Mental illness; Mood; Psychosocial problems; Nepal; Symptoms
References
- Liang T. Digital Support for Epidemic Prevention and Control. In: Handbook of COVID-19 Prevention and Treatment. 2020.
- McIntosh K. Coronavirus disease 2019 (COVID-19). Hirsch MS, Bloom A (Eds.). 2019.
- Knoll JL. Panic and Pandemics: The Return of the Absurd. Psychiatric Times. 2020.
- Ministry of health and population, Nepal. Coronavirus disease (COVID-19) outbreak: Updates and Resource materials.
- Country and Technical guidance- Coronavirus disease (COVID-19). 2019.
- Koirala BP. Institute of Health Sciences. Annual Report (2018-19) and Plan of Actions (2019-20).
- Shakya DR, Lamichhane N, Shyangwa PM, Shakya R. Nepalese psychiatric patients with armed-conflict related stressors. Health Renaissance. 2011; 9: 67-72.
- Shakya DR. Psychiatric emergencies in Nepal. Developing Mental Health. 2015; 2: 6-8.
- Shakya DR. The Nepal earthquake- use of a disaster to improve mental health literacy. Br J Psych Int. 2015; 13: 8-9. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/29093882
Similar Articles
-
Burnout and Related Factors in Caregivers of outpatients with SchizophreniaHatice Demirbas*,Erguvan Tugba Ozel Kizil. Burnout and Related Factors in Caregivers of outpatients with Schizophrenia. . 2017 doi: 10.29328/journal.hda.1001001; 1: 001-011
-
Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and GermanyJochen Hardt*,Lisa Weyer,Malgorzata Dragan,Wilfried Laubach. Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and Germany. . 2017 doi: 10.29328/journal.hda.1001003; 1: 015-022
-
Mindset kinetics and some depression status: A new quantitative model under biochemical - toxicology approach?Luisetto M*,Ghulam Rasool Mashori,Behzad Nili-Ahmadabadi,Farhan Ahmad Khan,Kausar Rehman Khan. Mindset kinetics and some depression status: A new quantitative model under biochemical - toxicology approach?. . 2018 doi: 10.29328/journal.ida.1001008; 2: 029-039
-
Problems shared in psychiatry helpline of a teaching hospital in eastern Nepal during COVID-19 pandemic lockdownDhana Ratna Shakya*. Problems shared in psychiatry helpline of a teaching hospital in eastern Nepal during COVID-19 pandemic lockdown. . 2020 doi: 10.29328/journal.ida.1001017; 4: 037-039
-
Psychological studies of stress experienced by seamen during a long-distance sea voyage#Mieczysław Plopa*. Psychological studies of stress experienced by seamen during a long-distance sea voyage#. . 2020 doi: 10.29328/journal.ida.1001019; 4: 049-054
-
Prevalence and measurement of anxiety and depression in nurses during COVID pandemic in NepalAyush Chandra*,Avinash Chandra,Nabina Sharma. Prevalence and measurement of anxiety and depression in nurses during COVID pandemic in Nepal. . 2020 doi: 10.29328/journal.ida.1001021; 4: 059-063
-
Burden and depressive symptoms in health care residents at COVID-19: A preliminary reportDaniela Betinassi Parro-Pires*,Sérgio Henrique de C Matias Barros,Fernanda Sabina HD Araújo,Daniel Zandoná Santos,Luiz Antônio Nogueira-Martins,Vanessa de Albuquerque Citero. Burden and depressive symptoms in health care residents at COVID-19: A preliminary report. . 2021 doi: 10.29328/journal.ida.1001024; 5: 005-008
-
Impact of amitriptyline on learning and memoryMfem CC,Seriki SA*. Impact of amitriptyline on learning and memory. . 2021 doi: 10.29328/journal.ida.1001025; 5: 009-015
-
Depression and anxiety in patients with suspected renal artery stenosisLudvig Hallberg*,Anders Gottsater,Anders Isaksson,Asa Westrin. Depression and anxiety in patients with suspected renal artery stenosis. . 2021 doi: 10.29328/journal.ida.1001026; 5: 009-015
-
Observation of telepsychiatry service in a teaching hospital of eastern Nepal during COVID-19 pandemicDhana Ratna Shakya*. Observation of telepsychiatry service in a teaching hospital of eastern Nepal during COVID-19 pandemic. . 2021 doi: 10.29328/journal.ida.1001027; 5: 025-028
Recently Viewed
-
Obstructive Pyelonephritis Due to Postoperative Ureteral Stricture: A Case ReportAyoub Mamad*,Mohammed Amine Elafari,Mohammed Amine Bibat,Midaoui Moncef,Amine Slaoui,Tarik Karmouni,Abdelatif Koutani,Khalid Elkhader. Obstructive Pyelonephritis Due to Postoperative Ureteral Stricture: A Case Report. J Clin Med Exp Images. 2026: doi: 10.29328/journal.jcmei.1001039; 10: 003-005
-
The motivational factors and adverse events experienced by healthy volunteers donating bone marrow for researchMirella Ejiugwo,Georgina Shaw,Frank Barry,Janusz Krawczyk,Veronica McInerney*. The motivational factors and adverse events experienced by healthy volunteers donating bone marrow for research. Int J Bone Marrow Res. 2019: doi: 10.29328/journal.ijbmr.1001010; 2: 089-096
-
Primary myelofibrosis is not primary anymore since the discovery of MPL515 and CALR mutations as driver causes of mono-linear megakaryocytic and dual megakaryocytic granulocytic myeloproliferation and secondary myelofibrosisJan Jacques Michiels*,Hendrik De Raeve. Primary myelofibrosis is not primary anymore since the discovery of MPL515 and CALR mutations as driver causes of mono-linear megakaryocytic and dual megakaryocytic granulocytic myeloproliferation and secondary myelofibrosis. Int J Bone Marrow Res. 2019: doi: 10.29328/journal.ijbmr.1001003; 2: 018-026
-
Pure Erythroid Leukemia: The Sole Acute Erythroid LeukemiaFauzia Shafi Khan*,Khalid Mahmood,Alia Ahmad. Pure Erythroid Leukemia: The Sole Acute Erythroid Leukemia. Int J Bone Marrow Res. 2017: doi: 10.29328/journal.ijbmr.1001001; 1: 001-005
-
European Clinical Laboratory, Molecular and Pathological (ECMP) criteria for prefibrotic JAK2V617F-Thrombocythemia and Polycythemia Vera versus MPL515- and CALR-Thrombocythemia and Myelofibrosis: From Dameshek to Michiels 1950-2018Jan Jacques Michiels*,Zwi Berneman,Wilfried Schroyens,Fibo W J ten Kate,King Lam,Hendrik De Raeve. European Clinical Laboratory, Molecular and Pathological (ECMP) criteria for prefibrotic JAK2V617F-Thrombocythemia and Polycythemia Vera versus MPL515- and CALR-Thrombocythemia and Myelofibrosis: From Dameshek to Michiels 1950-2018. Int J Bone Marrow Res. 2019: doi: 10.29328/journal.ijbmr.1001002; 2: 001-017
Most Viewed
-
Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trialSathit Niramitmahapanya*,Preeyapat Chattieng,Tiersidh Nasomphan,Korbtham Sathirakul. Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trial. Ann Clin Endocrinol Metabol. 2023 doi: 10.29328/journal.acem.1001026; 7: 00-007
-
Physical Performance in the Overweight/Obesity Children Evaluation and RehabilitationCristina Popescu, Mircea-Sebastian Șerbănescu, Gigi Calin*, Magdalena Rodica Trăistaru. Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001030; 8: 004-012
-
Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging PresentationKarthik Baburaj*, Priya Thottiyil Nair, Abeed Hussain, Vimal MV. Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging Presentation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001029; 8: 001-003
-
Exceptional cancer responders: A zone-to-goDaniel Gandia,Cecilia Suárez*. Exceptional cancer responders: A zone-to-go. Arch Cancer Sci Ther. 2023 doi: 10.29328/journal.acst.1001033; 7: 001-002
-
The benefits of biochemical bone markersSek Aksaranugraha*. The benefits of biochemical bone markers. Int J Bone Marrow Res. 2020 doi: 10.29328/journal.ijbmr.1001013; 3: 027-031

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."