More Information
Submitted: April 18, 2023 | Approved: October 14, 2025 | Published: October 15, 2025
How to cite this article: Blase K. Optimizing Treatment of Depression, Trauma, and Anxiety Disorders through Neurophysiological Interventions. Insights Depress Anxiety. 2025; 9(1): 025-027. Available from:
https://dx.doi.org/10.29328/journal.ida.1001046
DOI: 10.29328/journal.ida.1001046
Copyright license: © 2025 Blase K. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Self-control; HRV; HRVBiofeedback; PTSD; Depression; Anxiety; Vagal nerve; Psychophysiology
Optimizing Treatment of Depression, Trauma, and Anxiety Disorders through Neurophysiological Interventions
Kees Blasé*
Medical Physicist, Neuropsychologist, Netherlands
*Address for Correspondence: Kees Blasé, Medical Physicist, Neuropsychologist, Netherlands, Email: [email protected]
Depression, trauma, and anxiety disorders continue to be predominant causes of global disability, with typical therapies proving to be only marginally successful. Heart Rate Variability Biofeedback (HRVB) offers patients a self-regulation method that improves the flexibility of the autonomic nerve system via resonance breathing. Clinical research shows that training can significantly lower symptoms of sadness and PTSD, with improvements shown after 4 to 8 weeks. HRVB is inexpensive, non-invasive, and scalable, making it a promising supplementary therapy in psychiatry. Subsequent study ought to inform its incorporation into clinical protocols.
Depression, anxiety disorders, and trauma disorders are among the most common global mental health conditions. The World Health Organization (2023) states that over 300 million individuals have anxiety disorders and over 280 million individuals have depression [1]. Most of the world’s disability-adjusted life years (DALYs) originate in these two groups. These diseases are also directly related to increased disease of the heart, suicide, and chronic difficulties in employment and with social life.
Antidepressant drugs, cognitive behaviour therapy (CBT), and trauma-focused therapies are typical therapies that assist many individuals, but which also carry some well-advertised disadvantages. Approximately 30% – 40% of individuals with major depression do not respond at all or completely to drugs, and at the end of two years the reuptake rate following therapy may be 50%. Due to this, there is particular hunger for other therapies which are readily available, inexpensive, and do not interfere.
Heart Rate Variability Biofeedback (HRVB) has proved to be an effective adjunct therapy for autonomic nervous system (ANS) disorders. By training individuals to breathe at the resonate frequency, HRVB enables individuals to be activated through the vagus nerve, regain physiological balance, and become resilient to stress. What makes the HRVB unique in comparison to medicine is the fact that it provides the patient with the necessary tools for them to manage their own health. They can take the knowledge with them and carry it on even after the formal therapy is concluded. This complements the healthcare system’s current objectives quite well, which aim at emphasizing prevention, autonomy of the patient, and long-term resiliency.
Heart Rate Variability (HRV) is a neurophysiological marker of the autonomic nervous system (ANS). Decreased HRV indices are correlated with negative physical and psychological outcomes, especially depression, trauma, and anxiety [2-4]. More than 5000 studies have been published about HRV and HRVBiofeedback. Most of the studies are focused on HRV as a marker, for instance, as a predictor of physical outcomes [5,6]. In this article, the focus will be on HRV biofeedback as an additional treatment in the treatment of depression and anxiety.
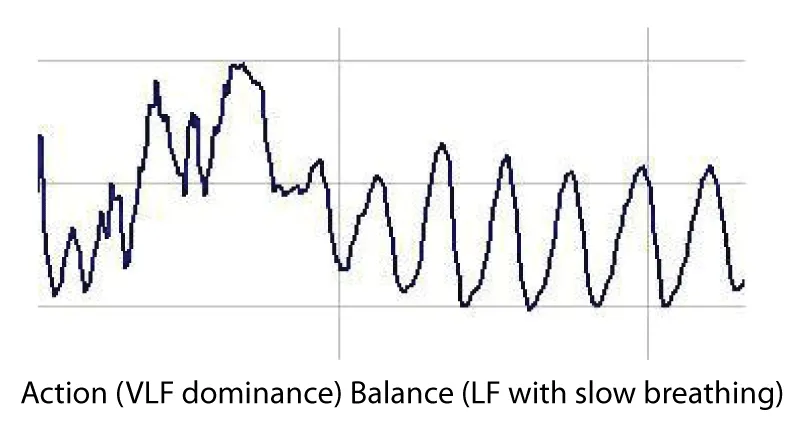
In clinical practice, HRV biofeedback is typically delivered in structured sessions of 30–45 minutes, conducted 2–3 times per week over an 8-week period. Patients are guided to breathe at their individual resonance frequency—usually between 4.5 and 6.5 breaths per minute—while monitoring HRV patterns in real time through visual or auditory feedback on devices such as the Balance Manager, Infinity, or StressEraser Pro (Figure 1).
Figure 1: HRV patterns (tachogram).
Each session begins with baseline HRV assessment, followed by paced breathing exercises. The feedback display allows patients to observe fluctuations across very low frequency (VLF), low frequency (LF), and high frequency (HF) bands. With repeated training, patients learn to shift from sympathetic dominance (Action/VLF) toward vagal activation (Calm/HF), or maintain balanced LF states. This process is believed to “rewire” autonomic reflexes, improving emotional regulation and stress resilience.
Beyond supervised sessions, patients are encouraged to practice daily home exercises for at least 15–20 minutes. Evidence suggests that adherence to daily practice enhances long-term outcomes, with significant reductions in depressive and anxiety symptoms typically observed after 4 weeks, and sustained improvements by 8 weeks of training.
Heart Rate Variability Biofeedback (HRVB) is a treatment in which patients learn self regulation of a physiological dysregulated vagal nerve function and restore the autonomic homeostasis [7-9]. HRVB affects cardiovascular homeostatic reflexes by increasing flexibility and recovery from fight or flight adaptive situations [8].
The Taskforce of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology formulated definitions of the various HRV metrics [2]. These are the international standards: HF, VLF, and LF.
VLF (very low frequency = 0.003 – 0.04 Hz), when measured over long time frames, has been interpreted as reflecting sympathetic activity (Action); LF (low frequency = 0.04 – 0.15 Hz) reflects the combination of sympathetic and vagal balance (Balance), though recent studies have questioned this interpretation and HF (high frequency = 0.15 – 0.4 Hz) is interpreted as reflecting vagal activity (Calm/sleepy).
We can describe this as ABC: Action, Balance, or Calm/Sleepy, where A indicates dominance of VLF (Action in the mind or body) B indicates Balance between sympathetic and vagal activity or LF and C indicates dominance of HF (Calm/sleepy).
When clients slow down breathing patterns in a resonance frequency (as shown above), they stimulate reflexes in the ANS that “rewire” this system to enhance ANS flexibility.
The new formula LF: (VLF+LF+HF) can be used as an index of the client’s success in achieving their training goals. This formula is used in HRVbiofeedback instruments, Balance Manager, and StressEraser Pro, clinically very relevant instruments.
A systematic review in 2021 about the efficacy of HRV biofeedback in the treatment of anxiety, depression, PTSD, and stress-related disorders [10] resulted in a total of 881 studies. The RCTs revealed significant clinical efficacy and better results compared with control conditions. Effects were visible after 4 weeks of training, but clinical practice in a longer daily self-treatment of 8 weeks is more promising.
After critical appraisal, 9 RCTs have been selected, as well as 2 other relevant studies. The RCTs with control groups, treatment as usual, muscle relaxation training, and a “placebo“-biofeedback instrument revealed significant clinical efficacy and better results compared with control conditions, mostly significant.
In the depression studies average reduction at the Beck Depression Inventory scale was 64% (HRVB plus Treatment as Usual (TAU) versus 25% (control group with Treatment As Usual), and 30% reduction (HRVB) at the PSQ scale versus 7% (control group with TAU).
In the PTSD studies average reduction on the BDI scale was 53% (HRVB plus TAU) versus 24% (control group with TAU) and 22% (HRVB) versus 10% (TAU) with the PCL scale. So the effect size is very relevant. Even with studies in groups from 26 to 60 participants, there is significant efficacy, so the effect size is very interesting.
That is why this neurophysiological additional treatment to create balance in the ANS is important in psychiatry [11], and maybe can be added to the guidelines of depression treatment and PTSD treatment. It is clinically very important that this additional treatment is used because of three different reasons.
1. Self-management and resilience by clients are important and relevant in the moment. A 2x reduction of depression and anxiety gives more efficient treatment in our healthcare. 3. Financially, it is important to keep the payment of our health care realistic.
In different studies has been shown that the dysregulated Vagal Nerve can be restored by HRVBiofeedback. HRV shows cardiovascular homeostatic reflexes by increasing flexibility and recovery from fight/flight adaptive situations [8,10]. At the moment, we see integration of HRV biofeedback in the Dutch Cardiology consortium, in Dutch Mental Health Care institutions, and in Stress Management trainings. Next steps are the implementation all over the world.
This can be realized with simple instruments, Balance Manager, Infinity, StressEraser Pro, and more, by breathing at a frequency resonating with heart rate variability. Feedback can be seen on the screen of the instruments: too much Activation (very low frequency), Balance (low frequency), and high frequency [12].
In the PTSD studies average reduction on the BDI scale was 53% (HRVB plus TAU) versus 24% (control group with TAU) and 22% (HRVB) versus 10% (TAU) with the PCL scale. These results are consistent with prior neuroscience research highlighting the role of trauma-related autonomic dysregulation in PTSD [13].
These findings are supported by smaller clinical investigations, such as a pilot study in patients with depression and PTSD, which reported significant improvements in HRV indices and mood symptoms after biofeedback training [14].
Heart Rate Variability Biofeedback (HRVB) is a promising adjunctive therapy for depression, PTSD, and anxiety disorders. By restoring autonomic balance through resonance breathing, HRVB provides clinically significant improvements, often doubling symptom reduction compared to standard care. Beyond short-term relief, it equips patients with practical self-regulation skills that enhance resilience and reduce relapse risk. As a non-invasive, low-cost, and scalable approach, HRVB is well suited for integration into mental health care, including digital platforms. Wider adoption may improve patient outcomes while supporting sustainable healthcare delivery.
Author contributions
The author was solely responsible for the conception, drafting, and revision of the manuscript.
Acknowledgment
The author gratefully acknowledges the contributions of previous researchers in the field of HRV biofeedback, whose work provided the foundation for this article.
- World Health Organization (WHO). Depression and anxiety fact sheet. Geneva: WHO; 2023 [cited 2025 Oct 14]. Available from: https://www.who.int/news-room/fact-sheets/detail/depression
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation. 1996;93(5):1043–65. Available from: https://pubmed.ncbi.nlm.nih.gov/8598068/
- Agelink MW, Boz C, Ullrich H, Andrich J. Relationship between major depression and heart rate variability: clinical consequences and implications for treatment. Psychiatry Res. 2002;113(1–2):139–49. Available from: https://doi.org/10.1016/s0165-1781(02)00225-1
- Karavidas MK. Heart rate variability biofeedback for major depression. Biofeedback. 2008;36:18–21. Available from: https://www.researchgate.net/publication/242455597_Heart_Rate_Variability_Biofeedback_for_Major_Depression
- Sloan RP, Shapiro PA, Bagiella E, Kuhl JP, Steinman RC, Gorman JM. Cardiac autonomic control and treatment of hostility: a randomized controlled trial. Psychosom Med. 2010;72(1):1–8. Available from: https://doi.org/10.1097/PSY.0b013e3181c8a529
- Lin IM, Fan SY, Yen CF, Yeh YC, Tang TC, Huang MF, et al. HRV biofeedback increased autonomic activation and improved symptoms of depression and insomnia in major depressive disorder. Clin Psychopharmacol Neurosci. 2019;17(2):222–32. Available from: https://doi.org/10.9758/cpn.2019.17.2.222
- Porges SW. The polyvagal theory: neurophysiological foundations of emotions, attachment, communication, and self-regulation. New York: W.W. Norton; 2011. Available from: https://www.scirp.org/reference/referencespapers?referenceid=1683048
- Gevirtz R. The promise of heart rate variability biofeedback: evidence-based applications. Biofeedback. 2013;41(3):110–20. Available from: https://doi.org/10.5298/1081-5937-41.3.01
- Blase KL, van Dijke A, Cluitmans PJ, Vermetten E. Effectiveness of HRV biofeedback in depression and PTSD. Tijdschr Psychiatr. 2016;58(4):292–300. Available from: https://pubmed.ncbi.nlm.nih.gov/27075221/
- Blase K, Vermetten E, Lehrer P, Gevirtz R. Neurophysiological approach by self-control of the ANS in depression, stress, and anxiety. Int J Environ Res Public Health. 2021;18(7):3329. Available from: https://doi.org/10.3390/ijerph18073329
- Lehrer PM, Gevirtz R, Simeon D, Shah K, Huseby R, Bhavsar J, et al. Heart rate variability biofeedback in psychiatric disorders: evidence and future directions. Appl Psychophysiol Biofeedback. 2020;45(3):207–22. Available from: https://doi.org/10.1007/s10484-020-09466-z
- Goessl VC, Curtiss JE, Hofmann SG. The effect of HRV biofeedback on stress and anxiety: a meta-analysis. Psychol Med. 2017;47(15):2578–86. Available from: https://doi.org/10.1017/s0033291717001003
- van der Kolk B. Clinical implications of neuroscience research in PTSD. Ann N Y Acad Sci. 2006;1071:277–93. Available from: https://doi.org/10.1196/annals.1364.022
- Siepmann M, Aykac V, Unterdörfer J, Petrowski K, Mueck-Weymann M. A pilot study on the effects of HRV biofeedback in patients with depression and PTSD. Appl Psychophysiol Biofeedback. 2008;33(4):195–201. Available from: https://doi.org/10.1007/s10484-008-9064-z