More Information
Submitted: April 05, 2022 | Approved: April 22, 2022 | Published: April 25, 2022
How to cite this article: Georgoulas-Sherry V. Predicting physical symptoms through expressions of loneliness and anxiety in individuals utilizing social media during SARS-CoV-2. Insights Depress Anxiety. 2022; 6: 011-017.
DOI: 10.29328/journal.ida.1001031
Copyright License: © 2022 Georgoulas-Sherry V. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Physical symptoms; Loneliness; Anxiety; Mental health; Social media
Predicting physical symptoms through expressions of loneliness and anxiety in individuals utilizing social media during SARS-CoV-2
Vasiliki Georgoulas-Sherry*
Saybrook University, 55 W Eureka St, Pasadena, CA 91103, USA
*Address for Correspondence: Vasiliki Georgoulas-Sherry, PhD, Saybrook University, 55 W Eureka St, Pasadena, CA 91103, USA, Email: [email protected]
The effect of the novel coronavirus (SARS-CoV-2) pandemic has produced significant health concerns negatively impacting individuals. As the ongoing and constantly changing nature of SARS-CoV-2 continues, the unique characteristics of this pandemic trend toward anxiety and loneliness as significant behavioral health outcomes. Furthermore, the SARS-CoV-2 pandemic has significantly impacted the utilization of social media platforms such as Twitter. Utilizing over 1.6 million tweets from approximately 988,760 Twitter users geolocated in Washington state from the University of Pennsylvania’s publicly available Twitter database (from March 2020 to March 2021), this study evaluated the impact of SARS-CoV-2 by using expressions of loneliness and anxiety to predict mental and physical symptoms. Bivariate correlations revealed expressions of loneliness were correlated to trouble breathing while expressions of anxiety were correlated to skin lesions, body aches, flu-like, seasonal cold, trouble breathing, nausea or diarrhea, fever, chills, and cough. Multiple multivariate linear regressions were completed, and a significant regression equation was found in predicting trouble breathing symptoms on expressions of loneliness and anxiety, however, the proportion of variance was 8% of the observed variation in the model. Further implications revealed the importance of understanding mental and physical well-being during a public health crisis as well as the use of social media platforms as primary and supplementary stimuli.
The effect of the novel coronavirus (SARS-CoV-2) pandemic has produced significant health concerns, both mental and physical, negatively impacting individuals in a multitude of ways, creating new hardships and barriers for individuals [1-7]. Even if individuals are not physically affected by SARS-CoV-2, the implications for behavioral health remain [7]. For example, a few studies have revealed that individuals who were 18 years and older reported negative mental health consequences such as a decrease in sleeping and eating, deterioration of chronic conditions, increase in psychological symptoms and behaviors, and increases in alcohol and drug consumption due to stress and concern over the pandemic [8-10]. In another study, Vahratian, et al. [7] study revealed that symptoms of a depressive or anxiety disorder increased in adults from August 2020 to February 2021, during the SARS-CoV-2 pandemic. As the ongoing and constantly changing nature of SARS-CoV-2 continues, the unique characteristics of this pandemic trend toward anxiety and loneliness as significant behavioral health outcomes [6,7]. This subsequently has led to behavioral health problems being considered critical and prevalent public health concerns, especially as the pandemic continues to considerably impact the community [1,4-7]. Furthermore, the SARS-CoV-2 pandemic has significantly impacted the utilization of social media platforms such as Twitter, especially during a time of social distancing, quarantining, and limited contact with others [2,3]. Twitter is a social media platform founded in 2006 which allows users to interact by sending, positing, and receiving short messages also known as ‘tweets.’ These platforms have begun to potentially offer a “window” into different individuals and communities, as a whole, and help forecast the long-term effects of SARS-CoV-2 [3]. Utilizing over 1.6 million tweets from approximately 988,760 Twitter users geolocated in Washington State from the University of Pennsylvania’s publicly available Twitter database, this study evaluated the impact of SARS-CoV-2 by using expressions of loneliness and anxiety to predict mental and physical symptoms. The main objective of the study is to evaluate how expressions of loneliness and anxiety can predict physical symptoms — utilizing bivariate correlations and multivariate linear regression models to assess these relationships.
Anxiety and loneliness
Anxiety has been defined as an unpleasant emotion categorized by feelings of apprehension, tension, dread, worry, distress, and uneasiness [7]. Anxiety has been shown to predict other mental illnesses, higher occurrences of irritable bowel syndrome and disease, asthma, coronary heart disease, stress, and inadequate work productivity and job performance. In addition, anxiety has been linked with worsened health outcomes, increased utilization of health care services, decreased cognitive functions, increased severity of symptoms of chronic disease, decreased quality of life, and more experiences of suicidal ideation and thoughts [2,5,7,11,12].
On the other hand, loneliness is a complex and multi-dimensional construct as it is defined as a feeling categorized by a lack of value, intimacy, or quality in social relationships and associations that typically occur, or because individuals might have fewer social associations than preferred [13-15]. Loneliness has been associated with an increased risk of multiple chronic conditions such as cardiovascular disease, hypertension, metabolic disorders, lung disease, increased psychological and behavioral problems, poor psychological well-being and functioning, morbidity, increased low self-esteem, depression, and suicidal ideation [16-18].
The behavioral health symptoms of anxiety and loneliness have been associated with one another; many studies have investigated these constructs together as they have overlapping qualities and a reciprocal relationship [2,6,17]. Loneliness has been directly linked to increased anxiety, including paranoia and psychosis, impaired cognitive processing, and poor self-reported health, and positively correlated to neuroticism and negatively correlated to extraversion and conscientiousness [13-15]. Anxiety has been shown to partially mediate the relationship between loneliness and paranoia and facilitate loneliness, alienation, and negative life events [11,17,19]. Both anxiety and loneliness have been associated with increased infection and hospitalization rates, poorer self-perception of health, negative effects on health and well-being, a significant risk for depression, and reduced life satisfaction [14-18].
Physical symptoms
Physical symptoms are defined as symptoms that are indicators of typical medical ailments and conditions and are not an actual medical or mental conditions; physical symptoms (e.g., aches, fatigue, and headaches) are typical day-to-day features of normal life and affect behavior in numerous ways [20,21]. Anxiety and physical symptoms have been shown to produce a reciprocal relationship [11,19,21]. In the short term, anxiety increases blood pressure, chest pain, breathing issues, heart rate and palpitations, irritability, and headaches; in the long term, anxiety can increase the risk of depression, muscle aches and other pains, and extreme fatigue, and just to name a few. The physical symptoms of back pain, abdominal pain, and headaches have shown to be the best predictors of anxiety in terms of physical symptoms [21]. In the long term, anxiety is associated with coronary artery disease, psoriasis, diabetes, and chronic obstructive pulmonary disease [21]. Furthermore, loneliness and physical symptoms have also been shown to produce a reciprocal association [14,16,20-24]. Specifically, loneliness has been linked with decreases in self-regulation, increases in non-healthy lifestyle choices (e.g., obesity, poor sleeping), and increases in physiological functions such as elevated cholesterol levels and systolic blood pressure. Loneliness also has predicted physical symptoms such as stomachaches and headaches, decreases in self-regulation, and increases in non-healthy lifestyle choices [20-24]. However, few studies examine how both loneliness and anxiety predict physical symptoms, especially during the pandemic, with the utilization of social media platforms to share these medical and physical concerns.
Social media
The SARS-CoV-2 pandemic has significantly impacted the utilization of social media platforms such as Twitter, especially during a time of social distancing, quarantining, and limited contact with others [2,3,17]. Specifically, social media platforms have afforded the opportunity for individuals to stay connected and maintain relationships while quarantining and remaining at home [17]. Due to this increase in social media use, social media platforms have begun to potentially offer a “window” into different individuals and communities, as a whole, and help forecast the long-term effects of SARS-CoV-2 [2,3,17]. As social media platforms continue to be more commonly used and grow, more research needs to be conducted to better understand how individuals are utilizing these types of apparatuses, and whether the use of social media platforms can act as primary and supplementary stimuli to better understand mental and physical well-being [2,3]. For example, in Guntuku, et al. [3], social media platforms predicted depression producing an area under the curve (AUC) of 0.72. Especially as the impact of SARS-CoV-2 continues to increase social media platform habits and usage, more must be known about individuals who utilize this social media platform to post on physical and mental symptoms. This study will utilize over 1.6 million tweets from approximately 988,760 Twitter users geolocated in Washington State from the University of Pennsylvania’s publicly available Twitter database, evaluating the impact of SARS-CoV-2 by using expressions of loneliness and anxiety to predict mental and physical symptoms.
Current study
As the ongoing SARS-CoV-2 pandemic continues to change and impact the U.S, we need to be able to assess the mental health impact, and more specifically, expressions of anxiety and loneliness; furthermore, there is a need to evaluate how expressions of loneliness and anxiety, during the SARS-CoV-2 pandemic, can predict physical symptoms, especially as loneliness and anxiety have both shown to correlate with physical and other mental health outcomes [2-7]. Lastly, as the SARS-CoV-2 impact on social media platform utilization continues to allow individuals to share feelings and emotions, solicit and provide social support, as well track day-to-day experiences, there is merit to better understanding the employment of social media platforms to help show the potentially important tool of social media platforms in passively measuring both mental and physical health. The main objective of the study is to evaluate how expressions of loneliness and anxiety can predict physical symptoms — utilizing bivariate correlations and multivariate linear regression models to assess these relationships.
Design
This study was an observational retrospective analysis of publicly available data on mental symptoms (expressions of anxiety and loneliness) and physical symptoms (skin lesions, body aches, fatigue, flu-like symptoms, seasonal cold, trouble breathing, nausea or diarrhea, loss of appetite, fever, changes in smell or taste, abdominal pain, chills, cough, and headache) that were posted by users geotagged to Washington state (n = 988,760) on the social media platform, Twitter between March 2020 to March 2021.
Materials
Publicly available tweet data posted between March 2020 to March 2021 were obtained from GitHub (i.e., a repository online hosting service) from a large publicly available data set retrieved by the University of Pennsylvania’s Center for Digital Health; the University of Pennsylvania’s Center for Digital Health tracks tweet data on self-reported mental and physical symptoms across the United States. This study employed only Twitter users geolocated in Washington state. While the publicly available tweet data set captures a variety of self-reported mental and physical symptoms, for this study, physical symptoms evaluated and collected by the University of Pennsylvania’s Center for Digital Health include “skin lesions”, “body aches”, “fatigue”, “flu-like symptoms”, “seasonal cold”, “trouble breathing”, “nausea or diarrhea”, “loss of appetite”, “fever”, “changes in smell or taste”, “abdominal pain”, “chills”, “cough”, and “headache”; the mental symptoms include “expressions of anxiety” and “expressions of loneliness.” The University of Pennsylvania’s Center for Digital Health; the University of Pennsylvania’s Center for Digital Health pulled approximately 4 million pandemic-related tweets using Twitter API each day.
Participants
This study utilized more than 1.6 million tweets from approximately 988,760 Twitter users geolocated in Washington state from the University of Pennsylvania’s publicly available Twitter database (from March 2020 to March 2021). No other demographic data (i.e., age, gender, race/ethnicity) were provided in this publicly available data set.
Procedure
Publicly available tweet data posted between March 2020 to March 2021 were obtained from GitHub from the University of Pennsylvania’s Center for Digital Health. The large publicly available data set was downloaded and utilized to predict physical symptoms through expressions of loneliness and anxiety in Twitter users geolocated in Washington state.
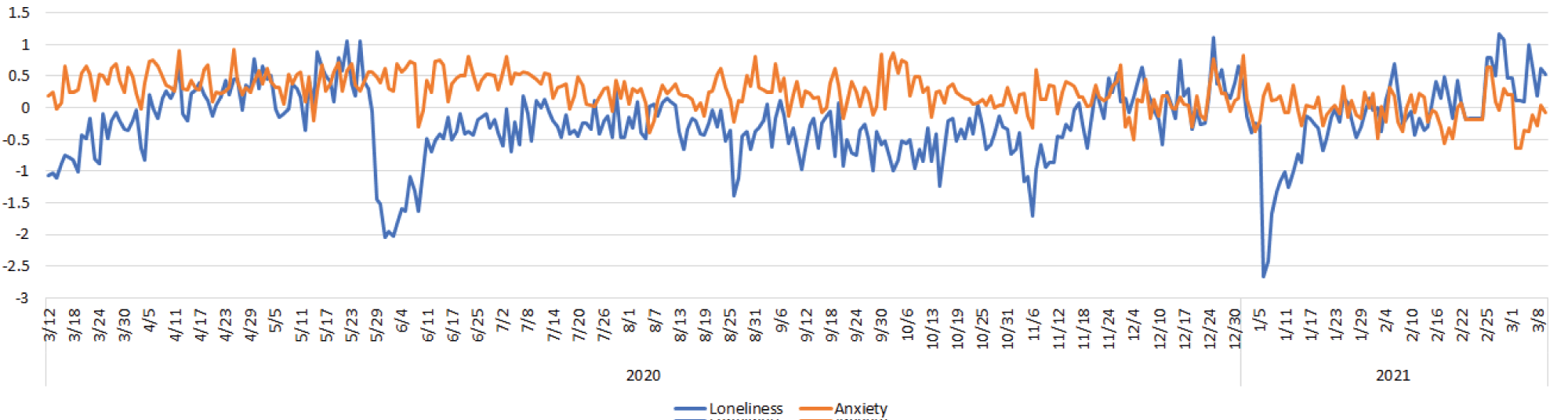
First, comparing expressions of anxiety and loneliness across duration of study, expressions of loneliness was not statistically significantly different in 2021 (M = -0.12, SD = 0.68) as compared with that in 2020 (M = -0.26, SD = 0.53) (Cohen’s d = 0.56; CI = [− 0.50, 0.02], p = 0.07, NS) and expressions of anxiety was higher in 2020 (M = 0.30, SD = 0.26) as compared with that in 2021 was higher (M = -0.03, SD = 0.28) (d = 0.26; CI = [0.96, 1.51], p < 0.001) (Figure 1).
Figure 1: Anxiety and Loneliness Across Duration.
Second, univariate associations between the mental symptoms (expressions of anxiety and loneliness) and physical symptoms (skin lesions, body aches, fatigue, flu-like symptoms, seasonal cold, trouble breathing, nausea or diarrhea, loss of appetite, fever, changes in smell or taste, abdominal pain, chills, cough, and headache) were evaluated using Pearson’s product-moment correlation coefficient. Bivariate correlations were used to evaluate the magnitude and direction of statistical relationship amongst the mental symptoms and physical symptoms) (Table 1). Findings revealed expressions of loneliness was correlated to trouble breathing (r = -.11, p = .03) while expressions of anxiety was correlated to skin lesions (r = .23, p < .001), body aches (r = .17, p = .002), flu-like (r = .20, p < .001), seasonal cold (r = .14, p = .007), trouble breathing (r = .25, p < .001), nausea or diarrhea (r = .11, p = .05), fever (r = .11, p = .04), chills (r = .13, p = .01), and cough (r = .19, p < .001). Expressions of loneliness and anxiety were not correlated to one another (r = .01, p = .80, NS).
| Table 1: Correlational Matrix of Study Constructs. | ||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
| 1. Skin Lesions | 1 | |||||||||||||||
| 2. Body Aches | 0.10 | 1 | ||||||||||||||
| 3. Fatigue | 0.10 | 0.05 | 1 | |||||||||||||
| 4. Flu-like | 0.23** | 0.39** | 0.12* | 1 | ||||||||||||
| 5. Seasonal Cold | 0.13* | 0.22** | 0.07 | 0.15** | 1 | |||||||||||
| 6. Trouble Breathing | 0.17** | 0.68** | 0.05 | 0.39** | 0.27** | 1 | ||||||||||
| 7. Nausea or Diarrhea | 0.06 | 0.58** | 0.04 | 0.25** | 0.12* | 0.54** | 1 | |||||||||
| 8. Loss of Appetite | 0.03 | 0.13* | 0.09 | 0.01 | 0.62** | 0.13* | 0.02 | 1 | ||||||||
| 9. Fever | 0.05 | 0.06 | 0.03 | 0.05 | 0.08 | 0.07 | 0.22** | 0.04 | 1 | |||||||
| 10. Changes in Smell or Taste | 0.15** | 0.08 | 0.15** | 0.06 | 0.14** | 0.12* | 0.11* | 0.23** | 0.05 | 1 | ||||||
| 11. Abdominal Pain | 0.02 | 0.00 | -0.01 | 0.04 | 0.08 | -0.01 | -0.01 | 0.00 | 0.02 | 0.04 | 1 | |||||
| 12. Chills | 0.13* | 0.16** | 0.09 | 0.16** | 0.10 | 0.08 | 0.08 | 0.02 | 0.06 | 0.10 | 0.06 | 1 | ||||
| 13. Cough | 0.26** | 0.08 | 0.07 | 0.15** | 0.18* | 0.16** | 0.04 | 0.01 | 0.08 | 0.16** | 0.02 | 0.09 | 1 | |||
| 14. Headache | 0.07 | 0.19** | 0.04 | 0.12* | 0.08 | 0.14** | 0.16** | -0.02 | 0.13* | 0.04 | 0.03 | 0.37** | 0.09 | 1 | ||
| 15. Loneliness | 0.02 | -0.05 | -0.02 | -0.07 | -0.03 | -.11* | -0.04 | -0.01 | -0.03 | -0.05 | 0.07 | 0.04 | -0.06 | 0.02 | 1 | |
| 16. Anxiety | 0.23** | 0.17** | 0.03 | 0.20** | 0.14** | 0.25** | 0.11* | 0.09 | 0.11* | 0.08 | 0.08 | 0.13* | 0.19** | 0.07 | 0.01 | 1 |
| *Correlation is significant at the 0.05 level (2-tailed); ** Correlation is significant at the 0.01 level (2-tailed). | ||||||||||||||||
Third, to examine the relationship between mental and physical symptoms, multiple multivariate linear regressions were completed. A significant regression equation was found in predicting skin lesions on expressions of loneliness and anxiety (F (2, 354) = 9.77, p < .001) with an R2 of 0.05, body aches (F (2, 354) = 5.61, p = .004) with an R2 of 0.03, flu-like symptoms (F (2, 354) = 8.32, p < .001) with an R2 of 0.05, seasonal cold symptoms (F (2, 354) = 3.84, p < .001) with an R2 of 0.02, trouble breathing symptoms (F (2, 354) = 14.68, p < .001) with an R2 of 0.08, chills (F (2, 354) = 3.47, p = .032) with an R2 of 0.02, and coughs (F (2, 354) = 7.42, p < .001) with an R2 of 0.04. Expressions of anxiety and loneliness did not predict fatigue (F (2, 354) = 0.21, p = .81, NS), nausea or diarrhea (F (2, 354) = 2.62, p = .11, NS), loss of appetite (F (2, 354) = 1.31, p = .27, NS), fever (F (2, 354) = 2.25, p = .11, NS), changes in smell or taste (F (2, 354) = 1.48, p = .23, NS), abdominal pain (F (2, 354) = 2.02, p = .13, NS), or headache (F (2, 354) = 1.02, p = .36, NS).
The main objective of the present study was to evaluate how expressions of loneliness and anxiety can predict physical symptoms — utilizing Bivariate correlations and multivariate linear regression models to assess these relationships. Findings from this study revealed that expressions of loneliness were correlated to trouble breathing. Expressions of anxiety were correlated to skin lesions, body aches, flu-like, seasonal cold, trouble breathing, nausea or diarrhea, fever, chills, and cough.
Findings from this study showed that expressions of loneliness were not significantly different in 2021 as compared with that in 2020, however, expressions of anxiety were higher in 2020 as compared with that in 2021. While current research has shown that the pandemic has yielded an epidemic of social isolation and loneliness amongst the U.S. adult population, findings from this study did not see a significant difference between 2020 and 2021. A lack of baseline data prevents the potential evaluation of this loneliness epidemic to either support or oppose the current analysis; however, this study does reveal that both years that have been impacted by SARS-CoV-2 did not differentiate in terms of loneliness. Expressions of anxiety were impacted in that 2020 showed higher levels of expressions of anxiety than 2021. These findings did mirror Jia, et al. [4] study that revealed that expressions of anxiety increased by 13% in the last part of 2020 (August to December) and then decreased in the first part of 2021 (January 2021 to June 2021) in the United States.
Results of this study show that expressions of loneliness and anxiety were not correlated to one another, which does not comport with previous research [15,22,24,25]. These findings were inconsistent to previous research that have shown that anxiety and loneliness have been associated to one another, and together, as they have overlapping qualities and a reciprocal relationship. Recent studies have shown mixed results between the use of social media and loneliness [14-18]. In one study, an increase use of Twitter showed a decrease in self-reported loneliness [18]. In another study, however, social media usage negatively affects well-being, as social anxiety and loneliness increase as social media usage also increases [17]. As research has shown that loneliness is associated to early mortality [14], poor mental health and depression [15], and increased health and social care costs [16], more work must be conducted to understand expressions of loneliness, especially as social media platforms are becoming more prevalent.
Furthermore, findings revealed that expressions of anxiety were correlated to skin lesions, body aches, flu-like, seasonal cold, trouble breathing, nausea or diarrhea, fever, chills, and cough while expressions of loneliness were only correlated to trouble breathing. However, expressions of anxiety were not correlated to fatigue, diarrhea, loss of appetite, changes in smell or taste, abdominal pain, and headache. Several multiple multivariate linear regression models were constructed to examine the model that can sufficiently describe the best fit. Multiple multivariate linear regressions revealed a significant regression equation was found in predicting trouble breathing symptoms on expressions of loneliness and anxiety, however the proportion of variance was 8% of the observed variation in the model.
Several limitations could have influenced the results of this study. First, this study utilized the social media platform, Twitter, which is composed of users that might not be representative of the population, and the results might not be generalizable beyond this sample. Social media platforms are typically for more technologically savvy individuals and this experience and environment might not fully represent the broader population. However, this study is important as this sample offers a unique illustration for investigating physical and mental symptoms, especially as social media platforms continue to expand. These types of platforms could potentially offer a distinct sample that would typically not be found in traditional research populations.
Second, this study did not obtain any baseline measures prior to the start of data collection However, the lack of baseline data is typical when evaluating disaster response related outcomes such as physical and mental health impacts. The use of publicly available social media platform data might allow for future evaluations of disaster data as there is higher likelihood that this data could be retrieved more readily. Real-time surveillance of social media posts, such as the Twitter data utilized in this study, can offer awareness into emergent issues of public concern especially following disasters, since there is potential for location specific data. Initial recognition of location-specific trends can produce inform distinct targeted public health interventions and improve preparedness in impending public health emergencies and adversities.
Lastly, this study lacked from a true experimental design. Research focusing on these mental and physical symptoms can benefit from non-correlational studies. While these symptoms were highly correlated with expressions of anxiety (not expressions of loneliness), as shown in this research, it would be interesting to see how these symptoms relate once variables are manipulated and isolated in an experimental study. Experimental research might produce meaningful results that might not be found in correlational research. Due to the limitations in this study, more work, especially with an experimental design, must be conducted to better understand how expressions of loneliness and anxiety can predict physical symptoms.
Implications
The effect of the SARS-CoV-2 pandemic has produced significant health concerns, both mental and physical, negatively impacting individuals in a multitude of ways, creating new hardships and barriers for individuals [1-7]. As the ongoing and constantly changing nature of SARS-CoV-2 continues, the unique characteristics of this pandemic trend toward anxiety and loneliness as significant behavioral health outcomes [8-10]. This subsequently has led to behavioral health problems being considered as critical and prevalent public health concerns, especially as the pandemic continues to considerably impact the community [5,7-10]. Better understanding, expressions of anxiety and loneliness can help support the future well-being and mental health, especially following emergencies and disasters.
As the health effects from a public health emergency like the SARS-CoV-2 pandemic go beyond the physical, taking an enormous mental toll in the immediate aftermath and the years following, more work must be done to better understand this impact. Studies like this one continue to enforce that mental health must be an integral part of the overall public health preparedness, response, and recovery system. Particularly, mental factors directly and indirectly influence individual and community risks, health, resilience, and the success of emergency response strategies and public health directives. Additionally, research like this showcases how mental health plays a critical role in community resilience and recovery from traumatic events, with a range of emotional, behavioral, physical, and cognitive responses. As the ongoing SARS-CoV-2 continues to change and impact the U.S, we need to be able to continue to assess the mental health impact.
Traditionally, much of research has been conducted through numerous experimental designs and measures. Utilizing social media can provide a “window” into different individuals and communities, as a whole. While surveys and assessments can offer a better understanding into various phenomena, social media platforms can offer more population-wide and real-time surveillance not assessed through typical methodologies. These types of platforms can provide insight into symptoms not otherwise measured as readily, such as well-being and mental and physical health. As social media platforms continue to allow individuals to share feelings and emotions, solicit and provide social support, and track day-to-day experiences, there is merit to better understanding the employment of social media platforms to passively measure both mental and physical health. While this study only evaluated expressions of loneliness and anxiety on physical symptoms, further research capacities can expand on its social media platform usage.
Assessing mental and physical symptoms, especially with location-specific data, can help address the behavioral health impacts of disasters and uniquely impact the cultivation of community resilience. Study endeavors like this one, which utilize real-time social media data, can present initial awareness and insight of declining mental health. For example, data, like the location-specific measures used in this study, can offer the opportunity for community-level responses and interventions. Work in this field can help support preparation for any type of emergency, facilitate and foster data-driven decision-making cultures, and monitor and mitigate the behavioral health impacts of emergencies. With location-specific data, this work can support population-level strategic planning and intervention, as well as inform forecasts used by health partners and state agencies for strategic planning, and interventions such as directing those experiencing traumas to appropriate resources. Lastly, time-sensitive, real-time data can help public health partners such as mental health providers and response teams respond quickly and appropriately to potential behavioral health outcomes of disasters. Further work in this area should be conducted in efforts to improve situational awareness during response, inform timely evidence-based decisions, and improve the efficiency of emergency management as the complexity and scope of emergencies/disasters continues to expand.
- Bryant-Genevier J, Rao CY, Lopes-Cardozo B, Kone A, Rose C, et al. Symptoms of depression, anxiety, post-traumatic stress disorder, and suicidal ideation among state, tribal, local, and territorial public health workers during the COVID-19 Pandemic—United States. March–April 2021. MMWR Morb Mortal Wkly Rep. 2021; 70: 947–952. PubMed: https://pubmed.ncbi.nlm.nih.gov/34197362/
- Cauberghe V, Van Wesenbeeck I, De Jans S, Hudders L, Ponnet K. How adolescents use social media to cope with feelings of loneliness and anxiety during COVID-19 lockdown. Cyberpsychol Behav Soc Netw. 2021; 24: 250–257. PubMed: https://pubmed.ncbi.nlm.nih.gov/33185488/
- Guntuku SC, Sherman G, Stokes DC, Agarwal AK, Seltzer E, et al. Tracking mental health and symptom mentions on twitter during COVID-19. J Gen Intern Med. 2020; 35: 2798–2800. PubMed: https://pubmed.ncbi.nlm.nih.gov/32638321/
- Jia H, Guerin RJ, Barile JP, Okun AH, McKnight-Eily L, et al. National and state trends in anxiety and depression severity scores amongst adults during the COVID-19 Pandemic—United States, 2020–2021. MMWR Morb Mortal Wkly Rep. 2020; 70: 1427–1432. PubMed: https://pubmed.ncbi.nlm.nih.gov/34618798/
- McKnight-Eily LR, Okoro CA, Strine TW, Verlenden J, Hollis ND, et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic—United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2021; 70: 162–166. PubMed: https://pubmed.ncbi.nlm.nih.gov/33539336/
- Palgi Y, Shrira A, Ring L, Bodner E, Avidor S, et al. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J Affect Disord. 2020; 275: 109-111. PubMed: https://pubmed.ncbi.nlm.nih.gov/32658811/
- Vahratian A, Blumberg SJ, Terlizzi EP, Schiller JS. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 Pandemic - United States, August 2020–February 2021. MMWR Morb Mortal Wkly Rep. 2021; 70: 490–494. PubMed: https://pubmed.ncbi.nlm.nih.gov/33793459/
- Barbosa C, Cowell AJ, Dowd WN. Alcohol consumption in response to the COVID-19 pandemic in the United States. J Addict Med. 2021; 15: 341–344. PubMed: https://pubmed.ncbi.nlm.nih.gov/33105169/
- Da Silva FR, Junior AHL, Brant VM, Lôbo ILB, Lancha LOP, et al. The effects of COVID-19 quarantine on eating and sleeping behaviors. Nutrire. 2020; 45: 25. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7523687/
- Kendzerska T, Zhu DT, Gershon AS, Edwards JD, Peixoto C, et al. The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review. Risk Manag Healthc Policy. 2021; 14: 575–584. PubMed: https://pubmed.ncbi.nlm.nih.gov/33623448/
- Kneer K, Reinhard J, Ziegler C, Slyschak A, Schiele M, et al. Serotonergic influence on depressive symptoms and trait anxiety is mediated by negative life events and frontal activation in children and adolescents. Eur Child Adolesc Psychiatry. 2020; 29: 691–706. PubMed: https://pubmed.ncbi.nlm.nih.gov/31422473/
- Løhre A, Lydersen S, Vatten LJ. School wellbeing among children in grades -10. BMC Public Health. 2010; 10: 1–7.
- Dalal N, Kathad A, Masurkar S, Pavithran S, Soumyanarayan T. Correlation studies between Big Five Personality traits, age and loneliness. Indian J Mental Health. 2018; 5: 32.
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspecti Psychol Sci. 2015; 10: 227–237. PubMed: https://pubmed.ncbi.nlm.nih.gov/25910392/
- Nangle DW, Erdley CA, Newman JE, Mason CA, Carpenter EM. Popularity, friendship quantity, and friendship quality: Interactive influences on children's loneliness and depression. J Clin Child Adolesc Psychol. 2003; 32: 546–555. PubMed: https://pubmed.ncbi.nlm.nih.gov/14710463/
- Mihalopoulos C, Le LKD, Chatterton ML, Bucholc J, Holt-Lunstad J, et al. The economic costs of loneliness: A review of cost-of-illness and economic evaluation studies. Soc Psychiatry Psychiatr Epidemiol. 2020; 55: 823–836. PubMed: https://pubmed.ncbi.nlm.nih.gov/31119308/
- O’Day EB, Heimberg RG. Social media use, social anxiety, and loneliness: A systematic review. Computers Human Behav Rep. 2021; 3: 100070.
- Pittman M. Creating, consuming, and connecting: Examining the relationship between social media engagement and loneliness. J Soc Media Soc. 2015; 4: 66–98. https://www.thejsms.org/index.php/JSMS/article/download/92/52
- Frasure-Smith N, Lesperance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry. 2008; 65: 62–71. PubMed: https://pubmed.ncbi.nlm.nih.gov/18180430/
- Bryan JL, Baker ZG, Tou RY. Prevent the blue, be true to you: Authenticity buffers the negative impact of loneliness on alcohol-related problems, physical symptoms, and depressive and anxiety symptoms. J Health Psychol. 2017; 22: 605–616. PubMed: https://pubmed.ncbi.nlm.nih.gov/26490626/
- Larson GE, Booth-Kewley S, Merrill LL, Stander VA. Physical symptoms as indicators of depression and anxiety. Mil Med. 2001; 166: 796–799. PubMed: https://pubmed.ncbi.nlm.nih.gov/11569444/
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006; 21: 152-164. PubMed: https://pubmed.ncbi.nlm.nih.gov/16594800/
- Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychol. 2009; 28: 354 –363. PubMed: https://pubmed.ncbi.nlm.nih.gov/19450042/
- Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010; 25: 132–140. PubMed: https://pubmed.ncbi.nlm.nih.gov/20230134/
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol Aging. 2006; 21: 140–151. PubMed: https://pubmed.ncbi.nlm.nih.gov/16594799/