Research Article
Burnout and Related Factors in Caregivers of outpatients with Schizophrenia

Hatice Demirbas1* and Erguvan Tugba Ozel Kizil2
1Gazi University, Faculty of Arts, Department of Psychology Teknikokullar, 06500, Ankara, Turkey
2Ankara University School of Medicine, Department of Psychiatry, Cebeci-Mamak, 06590, Ankara, Turkey
*Address for Correspondence: Hatice Demirbas, PhD, Gazi University, Faculty of Arts, Department of Psychology Teknikokullar, 06500, Ankara, Turkey, Tel: +90-312/ 2021345; Fax: +90- 312/ 2131235; Email: [email protected]
Dates: Submitted: 27 February 2017; Approved: 07 March 2017; Published: 09 March 2017
How to cite this article: Demirbas H, Ozel Kizil ET. Burnout and Related Factors in Caregivers of outpatients with Schizophrenia.Insights Depress Anxiety. 2017; 1: 001-011. DOI: 10.29328/journal.hda.1001001
Copyright License: © 2017 Demirbas H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Burnout; Schizophrenia; Caregivers
ABSTRACT
Objectives: Care of a person with schizophrenia involves multiple problems, possibly leading to burnout which is a culturally influenced phenomenon. The aim of this study was to investigate burnout and related factors in caregivers of outpatients with schizophrenia.
Methods: Subjects included in the study were 40 primary caregivers of outpatients with schizophrenia (15 males, 25 females) whom were assessed with the Maslach Burnout Inventory (MBI), the Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI). Patients were also administered the Calgary Depression Scale (CDS). Also, sociodemographic information about patients and their caregivers were taken. The significance of differences between two groups was determined by Mann-Whitney U-test. The relationships between the variables were evaluated by Pearson correlation analysis.
Results: No significant difference was found in the MBI subscale scores in terms of caregivers gender, marital status, and education, being a family member, having enough information about the illness and taking support during caregiving. Emotional Exhaustion and Personal Accomplishment subscale scores of the caregivers were significantly different in terms of patients’ adaptation to treatment or not (respectively; p=0.010, p=0.030). The MBI-Emotional Exhaustion scores revealed significant positive correlations with the BDI and BAI total scores. Also, the MBI- Depersonalization scores and the BAI scores were positively correlated.
Conclusions: Burnout levels in caregivers of patients with schizophrenia were lower when compared with other cultures. Only treatment compliance predicted burnout, while other factors were excluded. Therefore, professionals have to help to patients primarily adapt to their treatment.
INTRODUCTION
A couple of decades ago, hospitals or psychiatric clinics were in charge of caring for patients with schizophrenia, nowadays family has taken functions which were performed in the past by psychiatric hospitals. These changes bring along burden and negative changes in families’ quality of life. Family members are significantly stressed as a result of having one of them with schizophrenia [1]. Thus, caregivers’ burden and quality of life due to a family member’s mental illness has been increasingly documented [2-4]. These studies with schizophrenia showed that illness severity, caregiver’s relation to the patient, social and environmental support [5], and cost influence the burden of caregivers. Higher level of burden was associated with caregivers who have lower level of education [6], caregivers’ coping abilities, patient contact, being a patient’s parent [7,8], quality of life [9], as well as patient’s symptoms [10], total duration of illness, needs for hospital care, economic difficulty, patient’s violence toward the caregivers [11], personality factors [4,12], male gender, age of onset of disease, unemployment and marital status [7,13,14].
Care of a person with schizophrenia involves multiple burdens, possibly leading to burnout. In literature, there was number of studies about burn-out in the relatives of psychiatric patients. Burnout is often used to describe responses to strain involved in work with patients by professional caregivers [15]. It refers to a state of emotional exhaustion caused by excessive psychological and emotional demands made on helping people [16].
Maslach and Jackson, defined three dimensions of burn-out syndrome; emotional exhaustion, depersonalization (a cynical and uncaring reaction towards care-recipients) and (low) personal accomplishment [17,18].
Cuijpers and Stam [19] found that burden in general and emotional exhaustion were the aspects of subjective burden -psychological consequences for the family and relative’s mental health, subjective distress, and burnout- best predicted by objective burden-patient’s symptoms and behavior within the social environment and their consequences. Caregivers of patients with schizophrenia was related with being patients spouse, having anxiety about patient, straining on relationship with the patient, and lack of ability to cope with the patient’s behaviour. Angelmeyer et al. [20] compares partners of persons with schizophrenia and depression with nursing staff based on dimensions of burnout. No significant differences were found in the three dimensions of burn-out for the two groups of caregivers. About one fourth of the respondents in both groups showed a high degree of burnout. Male caregivers are seemingly more likely to experience the typical symptoms of burnout, namely: depersonalization, diminished personal accomplishment, and emotional exhaustion [21].
In Turkey, caregivers have no formal training. Because of lack of rehabilitation services, burnout on the relatives of caring for the patient is considerable and that the relatives’ well being and mental health may become seriously impaired. Additional research about burnout of caregivers with chronic mental illness can be beneficial for the enhancement of healthcare services provided to patients and their caregivers. The aim of this study was to investigate burnout and correlates of the burn-out and related factors in caregivers of outpatients with schizophrenia.
METHODS
Sample
This study is a cross-sectional study which is a research tool used to capture information based on data gathered for a specific point in time. It aims to provide data on the entire population under study. Consecutive outpatients under the care of Ankara University Psychiatry Clinic with a principal diagnosis of schizophrenia, and their respective caregivers constituted the sample population. They consist of 40 primary caregivers of the outpatients (15 males, 25 females) who live exclusively with the patient and who is involved with the everyday care of the patient at home. An inclusion criteria is that caregivers are not involved in the care of any other family members with any mental illness. Sociodemographic characteristics of the caregivers were given in Table 1. Mean age (±sd) of the caregivers was 49.5 (±15.0), aged 22-80 years.
| Table 1: Sociodemographic characteristics of the caregivers. | ||
| N | % | |
| Gender | ||
| Male | 15 | 37.5 |
| Female | 25 | 62.5 |
| Education | ||
| Primary school | 20 | 40.0 |
| High school | 13 | 32.5 |
| University | 7 | 17.5 |
| Marital status | ||
| Single | 10 | 25.0 |
| Married | 25 | 62.5 |
| Widowed/Divorced | 5 | 12.5 |
| Relation to the patient | ||
| Mother/Father | 23 | 57.5 |
| Sister/Brother | 8 | 20.0 |
| Spouse | 5 | 12.5 |
| Others | 4 | 10.0 |
| Employment status | ||
| Employed | 8 | 20.0 |
| Unemployed | 1 | 2.5 |
| Housewife | 17 | 42.5 |
| Retired | 11 | 17.5 |
| Not stated | 3 | 7.5 |
| Information about patient mental illness |
||
| Yes | 26 | 65.0 |
| No | 14 | 35.0 |
| Taking psychological support | ||
| Yes | 15 | 37.5 |
| No | 25 | 62.5 |
Patients were 21 women, and 19 men. Three clinicians evaluated the patients and their caregivers. All the outpatients were diagnosed with schizophrenia based on the DSM-IV-R criteria for an average of 14 years by psychiatrists. Exclusion criteria were having alcohol abuse or neurological disorders.
ASSESSMENT MEASURES
Maslach Burnout Inventory (MBI)
The MBI is a widely used self-rating scale for measuring hypothetical aspects of burnout syndrome. It consists of 22 items with a seven-point rating scale representing three aspects (emotional exhaustion, depersonalisation and personal accomplishment). For the emotional exhaustion and depersonalisation subscales, high mean scores reflect high levels of burnout [18]. The validation of the Turkish version was done by Ergin et al. [22]. The seven-point rating scale was decided to be inappropriate for the Turkish culture and the rating scale was reduced to a five-point rating scale. In this study, the items of the MBI were used with minor changes in the scale so that the term ‘recipient’ referred to the ‘the patient’ and ‘job’ referred to the ‘care giving’ similar to the manner performed in the study of Angermeyer et al. [20]. Cronbach’s alpha was 0.88 for the MBI in the present study.
The Beck Depression Inventory (BDI)
This is a self-rating scale determining the level of depression, consisting of 21 items, each containing four statements. It was originally developed by Beck [23] and adapted to the Turkish population by Hisli [24]. Higher scores in the BDI reflect a higher level of depression.
The Calgary Depression Scale for Schizophrenia (CDS)
The CDS was developed by Addington et al. [25] and adapted to the Turkish population by Aydemir et al. [26]. The Scale was specifically developed to assess the level of depression in schizophrenia. It consists of 9 items with 4 statements. It has been extensively evaluated in both relapsed and remitted patients and appears sensitive to change. In this study, Cronbach’s alpha was 0.86.
The Beck Anxiety Inventory (BAI)
BAI assesses the frequency of anxiety symptoms of caregivers [27]. Ulusoy et al. [28] translated the BAI into Turkish population. The BAI consists of 21 items, each describing a common symptom of anxiety. The respondent is asked to rate how much the person has been bothered by each symptom over the past week on a 4-point scale ranging from 0 to 3. The items are then summed to obtain a total score that can range from 0 to 63.
Procedure
The present study was approved by the Ankara University Psychiatry Clinic. Patients were recruited from the Psychiatry Clinic at Ankara University, Faculty of Medicine. The diagnoses of the patients were made by the psychiatrists. Each patient and the principal caregiver interviewed with face-to-face. The interview comprised a structured demographic and clinical inquiry from both patients and caregivers designed by the second author. Informed consent was obtained from the participants after giving information about the study procedure. Caregivers were assessed with the Maslach Burnout Inventory (MBI), the Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI). Patients were also administered the Calgary Depression Scale (CDS). The depression and anxiety scales are the most commonly used scales to assess emotional states in Turkey. Also, sociodemographic information about patients and their caregivers were collected. The assessments were conducted by the psychiatrists at period of the study.
Statistical Analysis
The significance of differences between two groups was determined by Mann–Whitney U-test and the differences between three or more groups were analysed by Kruskal–Wallis Anova. The relationships between the variables were evaluated by Pearson correlation coefficients where appropriate. A two-tailed alpha of 0.05 and 0.01 was used for all significance tests. Reliability of the tests was calculated with Cronbach’s alpha test.
The relationships among MBI subtests were analyzed by using multiple linear regressions. Relation to the patient, information about illness, taking support, patients’ adaptation to treatment, being parent, CDS, BDI, and BAI were taken as independent variables. Three separate regression models were tested for each of the subscales in which emotional exhaustion, depersonalization and personal accomplishment were taken as dependent variables. Statistical analyses were carried out using the software SPSS version 16.0.
RESULTS
About two thirds of the relatives were females. The majority of caregivers were married (62.5%) and housewives (42.5%). Caregivers were most frequently the parents of the patients (57.5%), but also included the siblings (20.0%), the spouse (12.5%), and others (10%). Number of caregivers who were not receiving support was high (62.5%). Most caregivers received low level of support from other available family members or other institutions. Caregivers (65%) thought that they had sufficient knowledge about schizophrenia.
Thirty of patients (75%) were diagnosed as paranoid schizophrenia, six of them (15%) were disorganised schizophrenia, one of them (2.5%) were residual schizophrenia, and three of them (7.5%) were undifferentiated schizophrenia. Their duration of illness changes from 1-38 years. Patients were being treated on an average of 13.88±8.48 years, ranged 3 to 30 years. The symptoms that caregivers had difficulty in coping were 29.4% negative symptoms, 29.4% hallucinations/delusions, 17.6% aggression and 8.8% other symptoms.
The correlations of the caregivers from the study measures were given in table 2.
| Table 2: The correlation coefficients of the study measures. | ||||||
| Study measures | CDS | BDI | BAI | MBI-EE | MBI-D | MBI-PA |
| CDS | 1.0 | |||||
| BDI | 0.286 | 1.0 | ||||
| BAI | 0.172 | 0.354* | 1.0 | |||
| MBI-Emotional Exhaustion(EE) | 0.242 | 0.378* | 0.411** | 1.0 | ||
| MBI-Depersonalisation(D) | 0.283 | 0.265 | 0.517** | 0.574** | 1.0 | |
| MBI-Personal achievement(PA) | 0.197 | 0.248 | 0.286 | 0.473** | 0.550** | 1.0 |
| *p<0.05, **p<0.01 | ||||||
The emotional exhaustion scores revealed significant positive correlations with the BDI and BAI total scores (r=0.378, p<0.05; r=0.411, p<0.01, respectively). When depression and anxiety level of caregivers increases the emotional exhaustion also increases. Also, the depersonalization scores and the BAI scores were positively and highly correlated (r=0.517, p<0.01). When anxiety level of caregivers increases, depersonalization increases. On the other hand, there were no significant differences between subscale scores of MBI and CDS total score.
There were no significant differences in the MBI subscale scores in terms of caregivers’ gender, marital status, education, employment status, relation to the patient, being a family member, having enough information about the illness, taking support during care giving, patients’ gender, patient’s adaptation to treatment and duration of illness.
It was found that the female caregivers reported higher emotional exhaustion (X=21.37) and depersonalization (X=21.67) scores than the male caregivers (X=18.89, X=18.32, X=19.21; respectively) in MBI. Although, no differences found among score of MBI on caregivers’ gender and relation to the patient, the highest score of exhaustion (X=23.44), and depersonalization (X=22.81) in MBI was found on caregivers who were sister/brother. Caregivers who were parent had higher score of all of the aspects of scores (X=20.37, X=20.30, X=18.65, respectively) in MBI.
The emotional exhaustion and personal accomplishment subscale scores of the caregivers were significantly different in terms of patients’ level of adaptation to treatment (respectively; p=0.010, p=0.030) (Table 3). The emotional exhaustion and personal accomplishment mean scores (X=30.50, X=29.07) of the caregivers whose patient shows low level of adaption to treatment were significantly different from the caregivers whose patient shows high level of adaptation to treatment (X=18.38, X=18.68).
| Table 3: The scores of the caregivers from the study measures. | |||
| MBI-Emotional Exhaustion | MBI-Depersonalisation | MBI-Personal achievement | |
| Patients’ gender | |||
| Female | 19.40 | 21.95 | 20.29 |
| Male | 21.70 | 18.89 | 20.74 |
| † | 0.532 | 0.392 | 0.903 |
| Caregivers’ gender | |||
| Female | 21.37 | 21.67 | 21.19 |
| Male | 18.89 | 18.32 | 19.21 |
| † | 0.522 | 0.370 | 0.609 |
| Care giver education | |||
| Primary school | 20.52 | 21.70 | 18.35 |
| High school | 21.58 | 20.85 | 26.46 |
| University | 18.43 | 16.43 | 15.57 |
| ‡ | 0.187 | 0.396 | 0.083 |
| Marital status | |||
| Single | 20.04 | 19.04 | 19.90 |
| Married | 22.15 | 23.45 | 23.10 |
| Widowed/Divorced | 19.50 | 21.90 | 18.30 |
| ‡ | 0.871 | 0.554 | 0.690 |
| Relation to the patient | |||
| Mother/Father | 20.37 | 20.30 | 18.65 |
| Sister/Brother | 23.44 | 22.81 | 26.88 |
| Spouse | 17.80 | 18.20 | 21.90 |
| Other | 18.75 | 19.88 | 16.62 |
| ‡ | 0.832 | 0.905 | 0.322 |
| Being parent | |||
| Parent | 20.37 | 20.30 | 18.65 |
| Not parent | 20.68 | 20.76 | 23.00 |
| † | 0.934 | 0.898 | 0.243 |
| Employment status | |||
| Employed | 17.69 | 20.25 | 21.81 |
| Unemployed | 6.50 | 8.00 | 16.50 |
| Housewife | 25.26 | 24.06 | 23.62 |
| Retired | 15.82 | 15.41 | 16.14 |
| Not stated | 22.83 | 23.83 | 16.67 |
| ‡ | 0.155 | 0.246 | 0.508 |
| Information about illness | |||
| Yes | 19.73 | 19.23 | 19.06 |
| No | 21.93 | 22.86 | 23.18 |
| † | 0.569 | 0.332 | 0.286 |
| Taking support | |||
| Yes | 19.97 | 22.00 | 20.80 |
| No | 20.82 | 20.80 | 20.32 |
| † | 0.822 | 0.828 | 0.900 |
| Patients’ adaptation to treatment | |||
| High level of adaptation | 18.38 | 19.29 | 18.68 |
| Low level of adaptation | 30.50 | 26.21 | 29.07 |
| † | 0.012* | 0.140 | 0.032* |
| İllness duration | |||
| 1-10 years | 21.25 | 19.25 | 21.78 |
| 11-38 years | 20.00 | 21.33 | 19.65 |
| † | 0.739 | 0.567 | 0.570 |
| *p< 0.05, Data are given as mean rank MBI: Maslach Burnout Inventory, †Mann-Whitney U-test, ‡ Kruskal-Wallis Anova |
|||
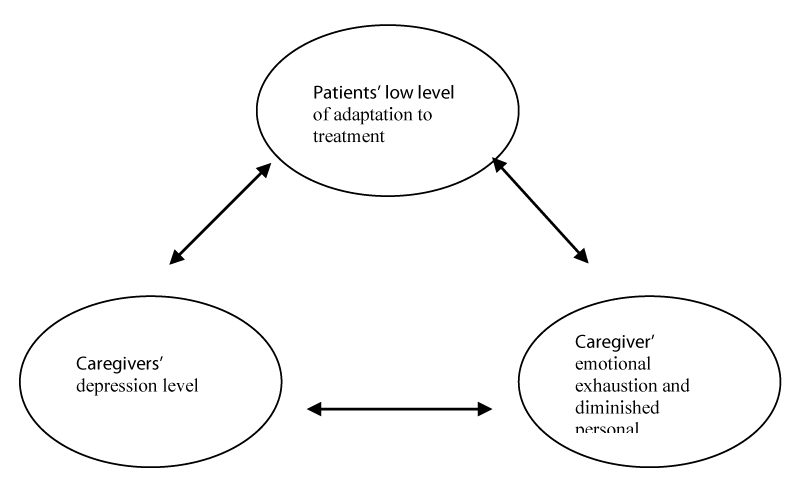
Three regression models were tested taking the each of the MBI subscores as the dependent variables. Significance and variance of the models and results of the linear regression analyses are shown in the (Table 4). To summarize the analysis results it can be said that patients’ low level of adaptation to treatment, being parent and high level of BDI score predicted a higher level of emotional exhaustion. Again being parent and high level of BAI score predicted a higher score from depersonalization. Moreover, being parent, patients’ high level of adaptation to treatment and high level of BDI score were related with lack of personal accomplishment. Depression was very important predictor of emotional exhaustion and lack of personal accomplishment. When depression was excluded from the model 1 and 3 as independent variable, regression coefficient was notably reduced from 0.39 to 0.30 for emotional exhaustion and from 0.47 to 0.32 for personal accomplishment. Mediation model of burnout for caregivers with schizophrenia was suggested in figure 1.
| Table 4: Results of multiple linear regression analysis. | |||
| Model 1 for Emotional Exhaustion (F(8,30)=2.36, p= 0.042, R²= 0.39) |
Model 2 for Depersonalisation (F(8,30)=3.63, p=0.005, R²= 0.49) |
Model 3 for Personal achievement (F(8,30)=3.36,p=0.007, R²= 0.47) |
|
| Beta | Beta | Beta | |
| Relation to the patient | -0.214 | -0.378 | -0.463 |
| Information about illness | 0.129 | 0.184 | 0.282 |
| Taking support | 0.141 | 0.039 | 0.200 |
| Patients’ adaptation to treatment | 0.345* | 0.253 | 0.396* |
| Being parent | 0.374** | 0.651* | 0.820** |
| CDS | -0.028 | 0.027 | -0.113 |
| BDI | 0.393* | 0.245 | 0.506** |
| BAI | 0.179 | 0.368* | 0.009 |
| *p<0.05, **p<0.01 | |||
DISCUSSION
The present study examined burnout and the factors related with burnout of caregivers of schizophrenia. This was the first study performing separate analyses for caregivers with schizophrenia. Burden and burnout are different phenomenon. Three Factor Model of Maslach and Jackson have been mostly emphasized in literature [18]. Underlying idea of the model is that burnout is a multidimensional syndrome consisting of three cognitive and affective components: emotional exhaustion, depersonalization, and lack of accomplishment. These 3 dimensions were assessed in this study. In literature, there were very limited studies with burnout. Therefore, study findings were generally compared with burden studies.
In this study it could not find any significant association between the patients’ and caregivers’ demographic characteristics which are in contrast to other studies [19]. This might be due to that fact that it was performed as cross-sectional analyses. Burnout scores of the caregivers are lower than other studies. This finding may be the result of the taking medicine regularly, being outpatients and mild-slight level of disease severity. These factors may be related with scores of burnout.
There were significant differential demographic associations with caregivers’ burden such as age, years of education, occupation of caregiver, and relationship of caregiver [29]. According to gender although there were no significant differences, it can be said that the female caregivers reported higher level of emotional exhaustion and depersonalization than the male caregivers probably because of the fact that they were mostly housewives (n=17, 42.5%) and had limited social resources and behaving with different social roles [11]. Therefore, family support should be taken from other available family members.
In this study, caregivers who were sisters/brothers and spouses have higher level of burnout than parents, but this finding did not reach the level of significance which might be due to high number of parent caregivers (n=23). On the other hand, in regression analysis, being parent was related to all dimensions of burnout. There were contradictory findings about relatives of patients in literature [30]. Some studies reported parents are more burdened than other relatives [31,32], others reported spouses are more burdened than parents [6,33]. These differences may emerge from characteristics of patients and caregivers. Winefield and Harvey [33] stated that parent and spouse caregivers had higher proportions of patient-related stress than other caregivers. Similar to this study finding, Kuwait study found that caregivers who were either children or spouses of patients had a tendency to have higher burden [6], emotional exhaustion [34] than other caregivers. In this study, number of spouses was limited. Therefore, in the future, a study with higher number of spouses, children and sisters/brothers of patients is needed.
The problems for caregivers when patients live with them included a very wide range of difficulties. It was found that the caregivers whose patients show low level of adaptation to treatment have higher emotional exhaustion. The emotional exhaustion is the central quality of burnout and represents the basic individual stress dimensions of burnout. It refers to feelings of being overextended and depleted emotional and physical resources. On the other hand, it is surprising that caregivers whose patients have high level of adaptation to treatment experience diminished personal accomplishment. Namely, caregivers were faced with illness-specific burnout. Symptoms (negative symptoms, hallucinations/delusions, and aggression) of patients may cause difficulties for caregivers as a result, they may experience burnout. Caregivers reported that patients’ symptoms which experience difficulties were 29.4% negative symptoms, 29.4% hallucinations/delusions, 17.6% aggression and 8.8% other symptoms. Kokurcan et al. [30] and Roick et al. [31] reported that higher positive and negative symptoms have an effect on burden of relatives. These findings agree with this study. In Turkey, professions give importance to decreasing the symptoms of patients with schizophrenia in the acute period. But this is not sufficient for decreasing the burnout. It is recommended that healthcare professions must be follow up the patients with schizophrenia regularly. Also, they must be given structured psycho educational interventions about their illness, psychopathology and disability [35], because of adaptation to their illness. The reorientation of families towards associations and the establishments of psychoeducational groups for them are two complementary measures that have proven effective in reducing family caregiver’s sufferings [36]. Kulhara et al. [35], found that structured psychoeducation about illness was significantly better than routine outpatient care on several indices including psychopathology, disability, caregiver-support and caregivers-satisfaction. One study stated that adapting to patients’ illness and learning how to cope with everyday problems might have reduced the number of mothers’ problems [34]. If the relative felt more able to cope with the patients’ behavior, the relatives’ burnout diminished [19]. Similar to that study, feelings of being emotionally overextended and exhausted by patients’ illness and feelings of incompetence and lack of achievement and productivity at care giving can cause to emotional exhaustion. Therefore, adapting to the patients’ illness might have reduced the caregivers’ emotional exhaustion and lack of personal accomplishment.
Family is one major source of support [37]. On the other hand, living with a psychiatric patient can negatively affect psychological and physical health of family members. Caregivers can experience psychological problems, such as anxiety and depression [11]. Regression analyses identified similar predictors for all dimensions of burnout which in part could be explained by relatively high correlation between these variables. One of the most interesting findings of the study is the relation between level of depression and anxiety, and burnout of the caregivers. Depression was very important predictor of emotional exhaustion and diminished personal accomplishment. When depression levels increase, the emotional exhaustion also increases, and personal accomplishment decreases. Only patients’ low level of adaptation to treatment predicts emotional exhaustion. One explanation of this that low level of patients’ adaptation to treatment lead to burn out and depression on caregivers. Lasebikan and Ayinde emphasized that caregivers are potential high risk group for mental disorders [29]. Magana et al. [38] found that higher levels of patients’ mental illness symptoms were predictive of higher levels of caregivers’ depressive symptoms. Patients who had higher level of symptoms may be low level of adaptation to treatment. Moreover, anxiety level was predictor and related with depersonalization. According to this study, anxiety level is related with emotional exhaustion but it was not predictor of emotional exhaustion. Depersonalization component of burnout represents the interpersonal context dimensions of burnout. It refers to a negative, callous, or excessively detached response to various aspects of the caregiving. When depersonalization increases also anxiety level increases. Consistent with these findings caregivers’ anxiety and depression levels were correlated with caregiver’s perceived family burden in Turkey [11]. Also, Aydin et al. [39] reported relationship between the severity of anxiety and depression symptoms, and quantity of daily life. Therefore, healthcare systems must give an importance to the psychological problems of caregivers. Because of over 80% of caregivers reported moderate to high level of subjective burden in one study [29].
Care of a person with schizophrenia involves multiple problems, possibly leading to burnout which is a culturally influenced phenomenon. In Turkey, caregivers with patients with schizophrenia have several difficulties in the absence of adequate support and education programs.
In clinical point of view, the present findings underline the necessity of putting more emphasis on adaptation to treatment of patient. Clinicians must be educating patients with schizophrenia about their illness, symptoms, importance of treatment, importance of regularly taking medicine, regular control by their doctors. As a result this education, may have accounted for improvements in both families and patients functioning and symptoms, rehospitalisation rates [40] and medical cost [36] will be decrease. Also, interventions provided by healthcare professionals will reduce caregivers’ depression and anxiety level. For this reason, caregivers of patients should also be screened and assessed with them by clinicians.
This study has some limitations. One of them is being cross-sectional. The other one is limited size of caregivers. Therefore, future studies may address burnout in caregivers of patients with different illnesses and risk factors of burnout may be studied in larger samples. The other limitation is that there was no control group. Economic condition is important, but in this study effect of the economic condition of caregivers and duration of caregiving were not evaluated. How many hours of contact with the patient which is related to burnout was not investigated.
As a conclusion, the present study revealed some important findings that the caregivers whose patients show low level of adaptation to treatment have higher emotional exhaustion. The following were significant predictors of burnout; patients’ low level of adaptation to treatment, being parent, higher depression and anxiety level. As a result, psychoeducation to patients about illness, taking support from other available family members and assessing the caregivers’ affection are very important for reducing burnout.
REFERENCES
- Martens L, Addington J. The psyhological well-being of family members of individuals with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2001; 36: 128-133. Ref.: https://goo.gl/cfDEMJ
- Caqueo-Urízar A, Gutiérrez-Maldonado J, Miranda-Castillo C. Quality of life in caregivers of patients with schizophrenia: a literature review. Health Qual Life Outcomes. 2009; 11: 84. Ref.: https://goo.gl/lWXmFr
- Heider D, Angermeyer MC, Winkler I, Schomerus G, Bebbington PE, et al. A prospective study of Quality of life in schizophrenia in three European countries. Schizophr Res. 2007; 93: 194-202. Ref.: https://goo.gl/6o8GTo
- Möller-Leimkühler AM, Obermeier M. Predicting caregiver burden in the first admission psychiatric patients. Eur Arch psychiatry Clin Neurosci. 2008; 258: 406-413. Ref.: https://goo.gl/XFhoVK
- Cechnicki A, Bielańska A, Hanuszkiewicz I, Daren A. The predictive validity of Expressed Emotions (EE) in schizophrenia. A 20-year prospective study. J Psychiatr Res. 2013; 47: 208-214. Ref.: https://goo.gl/GiRn5A
- Zahid MA, Ohaen JU. Relationship of family caregiver burden with quality of care and psychopathology in a sample of Arab subjects with scizophrenia. BMC Psychiatry. 2010; 10: 1-11. Ref.: https://goo.gl/6ncj0Y
- Roick C, Heider D, Bebbington PE, Angermeyer MC, Azorin JM, et al. Burden on caregivers of people with schizophrenia: comparison between Germany and Britain. Br J Psychiatry. 2007; 190: 333-338. Ref.: https://goo.gl/yBJ0Zw
- Marquez JA, Ramirez Garcia JI. Family caregivers' monitoring of medication usage: a qualitative study of mexican-origin families with serious mental illness. Cult Med Psychiatry. 2011; 35: 63-82. Ref.: https://goo.gl/frk0qx
- Parabiaghi A, Lasalvia A, Bonetto C, Cristofalo D, Marrella G, et al. Predictors of changes in caregiving burden in people with schizophrenia: a 3-year follow-up study in a community mental health service. Acta Psychiatr Scand. 2007; 437: 66-76. Ref.: https://goo.gl/p5xhpH
- Kate N, Grover S, Kulhara P, Nehra R. Relationship of caregiver burden with coping strategies, social support, psychological morbidity, and quality of life in caregivers of schizophrenia. Asian J Psychiatr. 2013; 6: 380-388. Ref.: https://goo.gl/Lu32bY
- Gulseren L, Cam B, Karakoc B, Tigit T, Danaci AE, et al. The Perceived burden of care and its correlates in schizophrenia. Turk Psikiyatri Derg. 2010; 21: 203-212. Ref.: https://goo.gl/RVTtCu
- Hjärthag F, Helldin L, Karilampi U, Norlander T. Illness-related components for the family burden of relatives to patients with psychotic illness. Soc Psychiatry Psychiatr Epidemiol. 2010; 45: 275-283. Ref.: https://goo.gl/C5rPtN
- \Igberase OO, Morakinyo O, Lawani AO, James BO, Omoaregba JO. Burden of care among relatives of patients with schizophrenia in midwestern Nigeria. Int J Soc Psychiatry. 2012; 58: 131-137. Ref.: https://goo.gl/TCzWGt
- Hosseini SH, Sheykhmounesi F, Shahmohammadi S. Evaluation of mental health status in caregivers of patients with chronic psychiatric disorders. Pak J Biol Sci. 2010; 13: 325-329. Ref.: https://goo.gl/LReezR
- Aström S, Waxman HM, Nilsson M, Norberg A, Winblad B. Wish to transfer to other jobs among long-term care workers. Aging. 1991; 3: 247-256. Ref.: https://goo.gl/ib4hDY
- Jackson SE, Schwab RL, Schuler RS. Toward an understanding of the burnout phenomenon. The Journal of Applied Psychology. 1986;71: 630-640. Ref.: https://goo.gl/Ub3hpA
- Köeske GF, Koeske RD. Construct validity of the Maslach Burnout Inventory: A critical review and reconceptualization. J Appl Behav Sci. 1989;25: 131-144. Ref.: https://goo.gl/YIRfQ9
- Maslach C, Jackson SE. The measurement of experienced burnout. J Occupational Behav. 1981; 2: 99-113. Ref.: https://goo.gl/xYnrGG
- Cuijpers P, Stam H. Burnout among relatives of psychiatric patients attending psychoeducational support groups. Psychiatr Serv. 2000; 51: 375-379. Ref.: https://goo.gl/bptMXz
- Angermeyer MC, Bull N, Bernert S, Dietrich S, Kopf A. Burnout of caregivers: a comparison between partners of psychiatric patients and nurses. Arch Psychiatr Nurs. 2006; 20: 158-165. Ref.: https://goo.gl/vFpcxR
- Hubbell L, Hubbell K. The burnout risk for male caregivers in providing care to spouses afflicted with Alzheimer's disease. J Health Hum Serv Adm. 2002; 25: 115-132. Ref.: https://goo.gl/j7etIW
- Ergin C. Doktor ve Hemşirelerde Tükenmişlik ve Maslach Tükenmişlik Ölçeği’nin Uyarlanması.In: Bayraktar R, Dag I, eds. VII. Ulusal PsikolojiKongresi Bilimsel Çalısmaları, Ankara: Türk Psikologlar Dernegi Yayını. 1992; 143-154.
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4: 561-571. Ref.: https://goo.gl/ZKj3xP
- Hisli N. Reliability and validity of Beck Depression Inventory in university students. Turk Psikoloji Derg. 1989; 23:3-13.
- Addington D, Addington J, Chissel B. A depression rating scale for schizophrenics. Schizophrenia Research. 1990; 3: 247-251. Ref.: https://goo.gl/Zt2BLe
- Aydemir O, Esen Danaci A, Deveci A, Icelli I. Reliability and validity of Turkish Calgary Depression Rating Scale. Arch Neuropsychiatr. 2000; 37: 82-86.
- Beck AT, Epstein N, Brown G. An Inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988; 56: 893-897. Ref.: https://goo.gl/MDnPvf
- Ulusoy M, Sahin NH, Erkmen H. Turkish version of the Beck Anxiety Inventory: Psychometric properties. J Cognit Psychother. 1998; 12:153-172.
- Lasebikan VO, Ayinde OO. Family burden in caregivers of schizophrenia patients: prevalence and socio-demographic correlates. Indian J Psychol Med. 2013; 35: 60-66. Ref.: https://goo.gl/6FHnle
- Kokurcan A, Yilmaz-Ozpolat AG, Gogus AK. Burnout in caregivers of patients with schizophrenia. Turk J Med Sci. 2015; 45: 678-685. Ref.: https://goo.gl/7mdk9J
- Roick C, Heider D, Toumi M, Angermeyer MC. The impact of caregivers characteristics, patients conditions and regional differences on family burden in schizophrenia: a longitudinal analysis. Acta Psychiatr Scand. 2006; 114: 363-374. Ref.: https://goo.gl/85mHNP
- Lowyck B, De Hert M, Peeters E, Wampers M, Gilis P, et al. A study of the family burden of 150 family members of schizophrenic patients. Eur Psychiatry. 2004; 19: 395-401. Ref.: https://goo.gl/BtAjiv
- Winefield HR, Harvey EJ. Needs of family caregivers in chronic schizophrenia. Schizophrenia Bull. 1994; 20: 557-566. Ref.: https://goo.gl/m3RbDX
- Wancata J, Freidl M, Krautgartner M, Friedrich F, Matschnig T, et al. Gender aspects of parents’ needs of schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2008; 43: 968-974. Ref.: https://goo.gl/mzivDB
- Kulhara P, Chakrabarti S, Avasthi A, Sharma A, Sharma S. Psychoeducational intervention for caregivers of Indian patients with schizophrenia: a randomised-controlled trial. Acta Psychiatr Scand. 2009; 119: 472-483. Ref.: https://goo.gl/ooMW6E
- Hodè Y. Prise en charge des familles de patients schizophre`nes:Family intervention for schizophrenia. Annales Me´ dico-Psychologiques. 2011; 169: 196-199. Ref.: https://goo.gl/VziNvH
- Sundara DC. A review of issues and concerns of family members of adult burn survivors. J Burn Care Res. 2011; 32: 349-357. Ref.: https://goo.gl/crn5RZ
- Magańa SM, Ramírez Garcia JI, Hernández MG, Cortez R. Psychological distress among Latino family caregivers of adults with schizophrenia: the roles of burden and stigma. Psychiatr Serv. 2007; 58: 378-384. Ref.: https://goo.gl/9K1ANQ
- Aydın A, Eker SS, Cangür Ş, Sarandöl A, Kırlı S. The Association of the Level of Caregiver Burden with the Sociodemographic Variables and the Characteristics of the Disorder in Schizophrenic Patients. Archives of Neuropsychiatry. 2009; 46: 10-14. Ref.: https://goo.gl/NFvO3f
- Réveillère C, Dutoit D, Beaune D, Nandrino JL, Goudemand M. Schizophrénie et famille. Contribution à l’étude et à la prévention de l’état de surcharge. Ann Méd Psychol. 2001; 159: 455-460. Ref.: https://goo.gl/6pIuSK